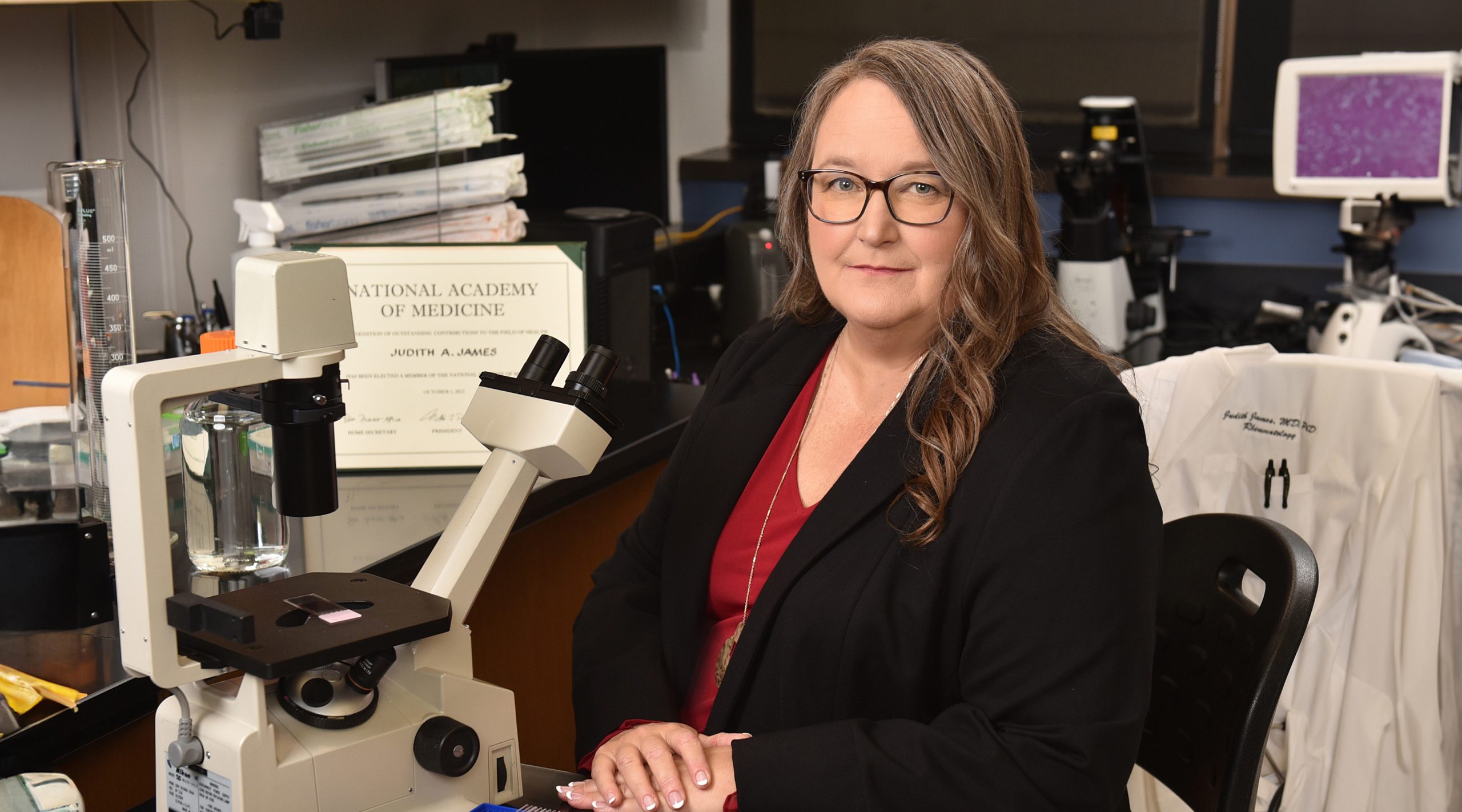
Judith A. James, M.D., Ph.D.
OMRF Executive Vice President & Chief Medical Officer
Professor and Program Chair
Arthritis & Clinical Immunology Research Program
Member, National Academy of Medicine; Lou C. Kerr Endowed Chair in Biomedical Research
Associate Vice Provost for Clinical & Translational Science
George Lynn Cross Professor of Research, Professor of Medicine, Professor of Pathology, Adjunct Professor of Microbiology and Immunology, University of Oklahoma Health Sciences Center
My 101
Systemic lupus erythematosus (SLE) is a debilitating disease that afflicts approximately nine times more women than men. SLE can affect nearly any organ in the body, including the skin, kidneys, heart, nervous system, and others.
Most organ damage in SLE arises from the actual disease process: the immune system produces autoantibodies that target and attack the body’s own cells and tissues. This process begins causing organ damage even before patients are diagnosed with SLE. Powerful immunosuppressants and steroids help SLE patients live longer, healthier lives, but they can also cause organ damage. Over time, organ damage from these two sources can lead to severe complications and early death. Our research is focused on addressing these problems.
In healthy individuals, the immune system maintains a balance between proteins that activate the immune system and proteins that inhibit the immune system. Our research shows that this balance is disrupted in the early stages of SLE development and becomes increasingly perturbed as patients approach clinical SLE diagnosis. Our ongoing research is defining the various pathways that can lead from early immune imbalances to SLE diagnosis. We also use mathematical modeling to pinpoint easily testable markers of SLE risk and this work has led to our participation in the first lupus prevention trial for high-risk individuals.
We also strive to improve treatment for patients who are already diagnosed with SLE. To understand why the disease waxes and wanes, we follow patients through relatively mild periods and more severe periods of disease activity called flares. We have identified immune imbalances that precede flares, and we are working with an industry partner to develop these results into a clinical test. We are also testing how these imbalances lead to flares. These studies could make it possible to safely reduce the use of unnecessary medications and to identify better directed treatments for SLE.
Research
My primary research focus is to decipher the complex genetic landscape of lupus and other autoimmune diseases. Like other autoimmune diseases, lupus is characterized by a production of autoantibodies that attack a wide variety of tissues and organs resulting in systemic inflammation and organ failure.
Our work has contributed significantly over the last decade to establish a strong genetic basis for lupus, and to provide important information about how genetic variations influence immune cell function to drive lupus development and progression. We use state-of-the-art high throughput sequencing technologies coupled with bioinformatics and functional analyses to systematically evaluate how genetic variations associated with lupus alter the genetic landscape and subsequent gene expression. Our overall objective is to develop a comprehensive view of the genetic landscape of lupus that can then be used to develop new or improved predictive and monitoring tools for patients with lupus.
Brief CV
Education
B.S., Oklahoma Baptist University (summa cum laude with honors), 1989
Ph.D., University of Oklahoma Health Sciences Center, 1993
M.D., University of Oklahoma Health Sciences Center, 1994
Honors and Awards
1988 Sir Alexander Fleming Scholar, OMRF
Outstanding Chemistry Student East Award, Oklahoma Baptist University
Outstanding Pre-Medical Student, Oklahoma Baptist University
1990, 1991 Travel Award Recipient, National Meeting American College of Rheumatology
1992, 1993 Outstanding Medical Student Award American College of Rheumatology
1992 Travel Award Recipient, National Meeting American Federation for Clinical Research
1994 Outstanding Student Award American College of Rheumatology
1994 Alpha Omega Alpha, Medical Honor Society
1996 The Merrick Award for Outstanding Research, OMRF
1997 Outstanding Presentation, Intern and Residents Day, University of Oklahoma Health Sciences Center
1998 Outstanding Oral and Poster Presentations, Intern and Residents Day, University of Oklahoma Health Sciences Center
2000 Merck Young Investigator Award
2000 Presidential Early Career Award for Scientists and Engineers
2001 Federation of Clinical Immunology Societies Junior Investigator Travel Award
2001 American Association of Immunologists Junior Faculty Travel Award
2001 Aesculapian Outstanding Medical Student Teaching Award Finalist Oklahoma University Health Sciences Center
2002 Byliner Award – Health Association for Women in Communications, Oklahoma City Chapter
2002 Henry Kunkel Society Membership
2003 Election to American Society of Clinical Investigation
2004 Edward L. & Thelma Gaylord Prize for Scientific Achievement
2005 OU Health Sciences Center Regent’s Award for Superior Research and Creative Activity
2007 Edmund L. Dubois, MD, Memorial Lectureship, Research and Education Foundation, American College of Rheumatology
2010 George Lynn Cross Research Professor, OUHSC
2013 Edward L. & Thelma Gaylord Prize for Scientific Achievement
2019 Evelyn V. Hess Award, Lupus Research Foundation
2019 Paul Klemperer, MD, Memorial Lectureship, American College of Rheumatology
2020 Stanley J. Korsmeyer Award, The American Society for Clinical Investigation
2022 Distinguished Basic/Translational Investigator Award, American College of Rheumatology
2022 Membership, National Academy of Medicine
Other Activities
Lupus Foundation of America National Medical Council – Grant Reviewer (1999 to present), Scientific Council Member (2016 to present)
Lupus Research Alliance Lupus Insight Prize Reviewer (2018, 2017)
Journal of Clinical Investigation Editor Selection Committee (2016)
The Judith and Stewart Colton Center for Autoimmunity, Chair, External Advisory Committee (2020 – present)
Acceleration Medicines Partnership (AMP) National Leadership Committee (2014 – present), Executive Committee (2016-present)
The American Society for Clinical Investigation Secretary-Treasurer and Council Member (2012 – 2015)
American College of Rheumatology (ACR) (June 2001), Section Chairman (2002-2003), Research and Education Foundation Chair (2006 – 2008), Abstract Reviewer for ACR Systemic Lupus Erythematosus-Clinical Category (2018 – present)
Lupus Clinical Investigators Network (LuCIN), Alliance for Lupus Research (ALR)/Lupus Research Institute (LRI) Steering Committee Member and Co-Chair of the Translational Studies Sub-Committee (2019)
Fellow, American College of Physicians (2019)
NIH National Institute of Allergy and Infectious Diseases (NIAID) Chairman, Sjögren’s Syndrome Working Group (2009 – present)
NIH National Institute of General Medical Sciences (NIGMS) National IDeA CTR PI Committee, (2014 – present)
Autoimmunity Centers of Excellence, NIH NIAID Clinical Chair of Steering Committee (2019 – present)
NIH National Institute Arthritis, Musculoskeletal and Skin Disease (NIAMS) R03 New Investigator Study Section (2001 – present)
NIH NIAMS Chairman, Council of Councils (2012 – 2014)
NIH NIAMS Scientific Council Member (2016 – 2021)
NIH NIAMS Chair, Council Planning Committee (2019 – 2021)
Ad Hoc Reviewer: VA Grant Review (National) (1997 to 2014)
Ad Hoc Reviewer: Nature Medicine, Journal of Immunology, Arthritis & Rheumatology, Journal of Clinical Investigation, Journal of Experimental Medicine, Genes and Immunity, Journal of Rheumatology, Scandinavian Journal of Immunology, Science & Translational Medicine, Annals of Rheumatic Disease, Science Signaling (1996 to present)
Graduate Program in Biomedical Sciences Advisory Committee Oklahoma University Health Sciences Center (2000 to present)
Lupus Foundation of Oklahoma Advisory Council (2000 to present)
Oklahoma Lupus Association, Inc. Board of Directors (2000 to present)
Memberships
American Society for Clinical Investigation
American College of Rheumatology
American Association of Immunologists
Federation of Clinical Immunology Societies
Oklahoma State Medical Association
American Medical Association
American Federation for Medical Research
Henry Kunkel Society
Oklahoma County Medical Society
American College of Physicians
Joined OMRF Scientific Staff in 1994
Publications
Recent Publications
Horisberger A, Griffith A, Keegan J, Arazi A, Pulford J, Murzin E, Howard K, Hancock B, Fava A, Sasaki T, Ghosh T, Inamo J, Beuschel R, Cao Y, Preisinger K, Gutierrez-Arcelus M, Eisenhaure TM, Guthridge J, Hoover PJ, Dall'Era M, Wofsy D, Kamen DL, Kalunian KC, Furie R, Belmont M, Izmirly P, Clancy R, Hildeman D, Woodle ES, Apruzzese W, McMahon MA, Grossman J, Barnas JL, Payan-Schober F, Ishimori M, Weisman M, Kretzler M, Berthier CC, Hodgin JB, Demeke DS, Putterman C, Brenner MB, Anolik JH, Raychaudhuri S, Hacohen N, James JA, Davidson A, Petri MA, Buyon JP, Diamond B, Zhang F, Lederer JA, Rao DA. Blood immunophenotyping identifies distinct kidney histopathology and outcomes in patients with lupus nephritis. J Clin Invest, 2025 June, PMID: 40536813
Wiley MM, Radziszewski M, Khatri B, Joachims ML, Tessneer KL, Stolarczyk AM, Yao S, Li J, Pritchett-Frazee C, Johnston AA, Rasmussen A, Anaya JM, Aqrawi LA, Bae SC, Baecklund E, Björk A, Brun JG, Bucher SM, Dand N, Eloranta ML, Engelke F, Forsblad-d'Elia H, Fugmann C, Glenn SB, Gong C, Gottenberg JE, Hammenfors D, Imgenberg-Kreuz J, Jensen JL, Johnsen SJA, Jonsson MV, Kelly JA, Khanam S, Kim K, Kvarnström M, Mandl T, Martín J, Morris DL, Nocturne G, Norheim KB, Olsson P, Palm Ø, Pers JO, Rhodus NL, Sjöwall C, Skarstein K, Taylor KE, Tombleson P, Thorlacius GE, Venuturupalli SR, Vital EM, Wallace DJ, Radfar L, Brennan MT, James JA, Scofield RH, Gaffney PM, Criswell LA, Jonsson R, Appel S, Eriksson P, Bowman SJ, Omdal R, Rönnblom L, Warner BM, Rischmueller M, Witte T, Farris AD, Mariette X, Shiboski CH, Sjögren’s International Collaborative Clinical Alliance (SICCA), Wahren-Herlenius M, Alarcón-Riquelme ME, PRECISESADS Clinical Consortium, Ng WF, UK Primary Sjögren’s Syndrome Registry, Sivils KL, Guthridge JM, Adrianto I, Vyse TJ, Tsao BP, Nordmark G, Lessard CJ. Variants in the DDX6-CXCR5 autoimmune disease risk locus influence the regulatory network in immune cells and salivary gland. Ann Rheum Dis, 2025 May, PMID: 40447495, PMCID: PMC12236377
Wagner CA, James JA. Risks and benefits of immunosuppressant withdrawal in systemic lupus erythematosus. Nat Rev Rheumatol, 2025 May, PMID: 40316794
Selected Publications
Dumas EK, Garman L, Cuthbertson H, Charlton S, Hallis B, Engler RJM, Choudhari S, Picking WD, James JA, Farris AD. Lethal factor antibodies contribute to lethal toxin neutralization in recipients of anthrax vaccine precipitated. Vaccine. 2017 Jun 8;35(26):3416-22. PMID: 28504191 PMCID: PMC5512426
Munroe ME, Vista ES, Merrill JT, Guthridge JM, Roberts VC, and James JA. Pathways of impending disease flare in African-American systemic lupus erythematosus patients. J Autoimmun. 2017 Mar;78:70-8. PMID: 28162788 PMCID: PMC5340190
Aberle T, Bourn RL, Munroe ME, Chen H… and James JA. 2017. Clinical and serological features distinguish patients with incomplete lupus classification from systemic lupus erythematosus patients and controls. Arthritis Care Res (Hoboken). 2017 Jan 24. PMID: 28118528 PMCID: PMC5524597
Munroe ME, Young KA, Kamen DL, Guthridge JM…and James JA. Soluble Mediators and Clinical Features Discern Risk of Transitioning to Classified Disease in Relatives of Systemic Lupus Erythematosus Patients. Arthritis Rheumatol. 2017 Mar;69(3):630-42. PMID: 27863174 PMCID: PMC5329053
James JA, Gross T, Scofield RH, Harley JB. Immunoglobulin epitope spreading and autoimmune disease after peptide immunization: Sm B/B'-derived PPPGMRPP and PPPGIRGP induce spliceosome autoimmunity. J Exp Med. 1995 181(2):453-61. PMID: 7530756 PMCID: PMC2191871
McClain MT, Heinlen LD, Dennis GJ, Roebuck J… and James JA. Early events in lupus humoral autoimmunity suggest initiation through molecular mimicry. Nat Med. 2005 11(1):85-9. PMID: 15619631
Contact
Arthritis & Clinical Immunology Research Program, MS 53
Oklahoma Medical Research Foundation
825 N.E. 13th Street
Oklahoma City, OK 73104
Phone: (405) 271-4987
Fax: (405) 271-7063
E-mail: Judith-James@omrf.org
For media inquiries, please contact OMRF’s Office of Public Affairs at news@omrf.org.
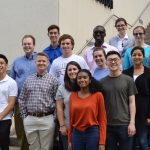
Lab Staff
Harini Bagavant, Ph.D.
Research Associate Professor
Melissa Munroe, Ph.D.
Research Associate Professor
Kenneth "Ken" Smith, Ph.D.
Research Associate Professor
Carla Guthridge, Ph.D.
Staff Scientist
Alexandre Cammarata, Ph.D.
Scientific Medical Writer
Ola Bylinska
Postdoctoral Scientist
Cathy Velte
Manager Core Faculty
Marci Beel
Manager Laboratory
Camille Anderson
Senior Technical Specialist
Timothy "Tim" Gross
Senior Technical Specialist
Xana Howard
Data Analyst
Zoe Reed
Data Analyst
Yi-Mei "Mei" Cheng
Research Technician IV
Randi Thompson
Research Technician IV
Dawn Updike
Research Technician IV
Kathleen Norris
Research Technician III
Eleanor Shore
Research Technician I
Kevin Thomas
Graduate Student
Sarah Hamilton
Business Administrator
Mary Flynn
Senior Grants Specialist
Veronica Gregory
Administrative Assistant IV
Clinic Staff
Cristina Arriens, M.D.
Clinical Associate Member
Nancy Redinger
Associate Director of Clinical Activities
Teresa Aberle
Physician Assistant
Victor Nguyen, PharmD.
Pharmacist
Christine Dresel, PharmD.
Pharmacist
Fredonna Carthen
Clinical Trial Project Administrator
Kallena Haynes
Clinical Research Associate
Elizabeth "Liz" Brouchoud
Clinical Research and Regulatory Specialist
Lena Fuentes
Clinical Research Coordinator
Judy Goodman
Clinical Research Coordinator
Faith Bullard
Clinical Trials Budget and Contract Analyst
Bridget Parrish
Research/Medical Communications Specialist
Stanley "Stan" Kamp
Research Technician IV
Jeffery "Jeff" Turner
Senior Clinical Research Technician
Crystal Ellis
Phlebotomist/Medical Assistant
Miranda Early
Medical Assistant
Teshala Moss
Medical Assistant
Noemi Hernandez
Patient Access Representative
News from the James lab

Each week, OMRF Chief Medical Officer Dr. Judith James opens “Adam’s Journal” to answer a medical question from Adam Cohen, OMRF’s senior vice president & general counsel. Adam’s Journal I vaguely remember hearing about RSV in the past, but only as an illness that affects infants. Now, I commonly hear it discussed as a threat […]

Each week, OMRF Chief Medical Officer Dr. Judith James opens “Adam’s Journal” to answer a medical question from Adam Cohen, OMRF’s senior vice president & general counsel. Adam’s Journal As we often do when we get together, my sister and I recently found ourselves in a friendly competition. This one was to see if we […]

March Today, just 1 in 5,000 experimental compounds proves safe and effective enough to reach patients. For new drugs, the road to hospitals and clinics is steep and long. Researchers screen countless promising compounds, but they choose only a few to begin clinical trials. Of those selected, roughly 9 out of 10 will fail. For that […]

Each week, OMRF Vice President of Research Dr. Rod McEver opens “Adam’s Journal” to answer a medical question from Adam Cohen, OMRF’s senior vice president & general counsel. Adam’s Journal Here’s a question from a reader: Dear Dr. McEver, I got my fourth Covid vaccination in September. I am at high risk because of my […]
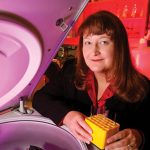
Election to the National Academy of Medicine is but the latest first for Dr. Judith James Dr. Judith James can’t remember not wanting to be a doctor. As a 5-year-old, James, who had severe asthma, shared her career intentions with her pediatrician. “He said if I wanted to become a nurse, he would be happy […]

OMRF’s education programs enjoyed a record summer in 2022. For most students, summer means late nights, lake days and snooze buttons. But for those who spend the dog days in OMRF’s labs, it’s mice, pipettes and data analysis. Despite the obvious appeal of a lazy few months between semesters, in recent years, OMRF has seen […]
The new millennium began with a bang at OMRF, as Dr. Jordan Tang, above, and his research team identified and cloned the enzyme believed to cause Alzheimer’s disease. Soon after, the OMRF scientists designed an inhibitor that stopped the enzyme in its tracks. The discoveries led to the development of an experimental drug acquired by […]
When Dr. William Thurman, above, took the helm of OMRF, he brought the lab coat he’d worn since his days training as a pediatric oncologist. That powder-blue garment, along with the bow ties he favored, would become synonymous with OMRF throughout the 1980s (and most of the 1990s). But his sartorial flourishes would prove the […]

When Dr. Matlock Jeffries began his first day of work at OMRF in August, it may have been the smoothest transition in the foundation’s history. That Monday morning, he entered the same lab where he’d been studying osteoarthritis for the previous four years. Only now, he’d be doing it as a member of OMRF’s scientific […]

You simply couldn’t find a scientist who was studying Covid-19 in 2019. Which makes sense, because it wasn’t until the final day of that year that China reported its first cluster of cases to the World Health Organization. In the months that followed, countless researchers pivoted to tackle the novel coronavirus that had emerged as […]
When a team of OMRF scientists set out to improve the anthrax vaccine, they started with a theory everybody thought would work: Break apart the toxins so they can’t enter cells. Problem solved. But things don’t always work as expected. In fact, the theory doesn’t work at all, according to a paper by OMRF’s Darise […]

The National Institutes of Health has awarded two grants worth a total of $26.3 million to OMRF for research into anthrax and to help train new scientists. Each grant will allow scientists to continue research started in 2004 and 2005 and keep them working through 2014 on several interconnected projects. In the first project, a $14.5 […]
Vitamin D has long been renowned for its role in creating strong bones. But research from OMRF suggests that the vitamin could also play an early role in autoimmune diseases such as lupus. OMRF researcher Judith James, M.D., Ph.D., and Lauren Cole, a graduate student in James’s lab, have found that in people who are […]
For many students, summer marks a time for rest and relaxation. For sailboats and sunscreen, beachcombing and barbecues. But don’t tell that to a dozen of Oklahoma’s top high school and college science students. As Sir Alexander Fleming Scholars at the Oklahoma Medical Research Foundation, they’ve opted to trade swimsuits for lab coats so they […]
OMRF has named 12 Oklahoma high school and college students as Sir Alexander Fleming Scholars for 2009. The students, chosen from a statewide pool of applicants, will comprise the 54th class of Fleming Scholars at OMRF. This year’s class will spend June and July working in laboratories with senior-level OMRF scientists on ongoing research projects. […]
The Oklahoma Medical Research Foundation is now accepting applications for its 2009 Sir Alexander Fleming Scholar Program. The application deadline is Feb. 1. High school seniors, as well as college freshmen, sophomores and juniors, are eligible to apply for the scholarships. Students selected as Fleming Scholars will work side-by-side in a laboratory with a senior-level […]
Nobody ever said fighting a disease couldn’t be fun. Since 2001, DeeAnn Simpson has organized the Eastern Star Bike Ride to increase awareness of multiple sclerosis and to raise funds to research the disease at the Oklahoma Medical Research Foundation. And at this year’s edition of the ride, which takes place on Saturday, Simpson hopes […]
The Oklahoma Medical Research Foundation has named nine Oklahoma science students as Sir Alexander Fleming Scholars for 2008. Nearly 100 applicants from high schools and colleges throughout Oklahoma competed for the prestigious program, which has launched the careers of physicians and researchers for more than a half-century. Since 1956, the Fleming Scholar Program has provided […]
The American College of Rheumatology has awarded Oklahoma Medical Research Foundation researcher Judith James, M.D., Ph.D., the 2007 Edmund L. Dubois Memorial Achievement Award. The prize is presented each year to an outstanding investigator in the field of lupus research. James was honored as a result of her groundbreaking work in predicting lupus, a disease […]
The Oklahoma Medical Research Foundation is accepting applications for its 2008 Sir Alexander Fleming summer scholarship program. The program lets students enhance their research skills by working alongside world-class scientists for eight weeks in OMRF’s state-of-the art laboratories. The application deadline is February 1. “The Fleming scholar program provides a phenomenal experience to young people […]
The National Institutes of Health has awarded the Oklahoma Medical Research Foundation $2.66 million to establish the Oklahoma Rheumatic Disease Research Cores Center. The grant, which will be awarded over a five-year period, will fund studies aimed at developing a better understanding of health problems characterized by pain in the muscles and joints. The project […]
Growing up, Judith James rarely passed up an episode of Star Trek. From her living room in Pond Creek, the future M.D./Ph.D. sat transfixed as Captain Kirk, Mr. Spock and the crew of the U.S.S. Enterprise boldly went where no man had gone before. For the future physician and medical researcher, the workings of the […]
For the past six years, DeeAnn Simpson has watched from the sidelines as bicyclists peddled in a charity ride for multiple sclerosis research at the Oklahoma Medical Research Foundation. This year, though, Simpson, the event’s organizer, also plans to hop on her own bike to join in the fight against MS. “My sons and I […]
Their peers may spend much of June, July and August sleeping late and lounging by the pool, But for a dozen of Oklahoma’s most talented high school and college science students, summer will mean donning lab coats and safety goggles in laboratories at the Oklahoma Medical Research Foundation. OMRF today announced its 2007 class of […]
The cover story in the current issue of Scientific American highlights a research study led by scientists at the Oklahoma Medical Research Foundation. The article, “Predicting Disease,” cites a study about predicting lupus and autoimmune diseases led by OMRF’s Judith James, M.D., Ph.D., and John Harley, M.D., Ph.D. The Scientific American article focuses on the […]
Judith James, M.D., Ph.D., of the Oklahoma Medical Research Foundation has been selected to present at the world’s largest interdisciplinary science forum this weekend. As one of four speakers on an international panel, James will present the latest scientific data on “Predicting Autoimmune Disease” at the annual meeting of the American Association for the Advancement […]
Nearing the mid-point of an historic five-year research project, the Oklahoma Medical Research Foundation announced today that it is making important strides toward developing more effective vaccines and treatments for the deadly infectious disease anthrax. In a study involving 120 military personnel, Judith James, M.D., Ph.D., Sherry Crowe, Ph.D., and Darise Farris, Ph.D., have identified […]
Oklahoma Medical Research Foundation scientist John Harley, M.D., Ph.D., has been named the inaugural recipient of a mentoring award from the nation’s leading rheumatology organization. Harley will be honored in Washington D.C. during the 70th Annual Scientific Meeting of the American College of Rheumatology (ACR) Research and Education Foundation. The new Excellence in Investigative Mentoring […]
The National Institutes of Health (NIH) has recognized the exemplary work of Oklahoma Medical Research Foundation scientist John Harley, M.D., Ph.D., with its prestigious MERIT (Method to Extend Research in Time) award. The multi-year award will provide more than $1.8 million to fund Harley’s research on the genetics of the autoimmune disease lupus. According to […]
The National Institutes of Health has awarded the Oklahoma Medical Research Foundation a $9.16 million grant to train junior scientists and build research infrastructure at OMRF. The five-year award will fund the work of five junior scientists and provide operating support for core facilities at the foundation. “This is yet another important step in the […]
The National Institutes of Health has awarded the Oklahoma Medical Research Foundation $8.132 million to study the influenza vaccine. The five-year project will examine why the vaccine does not protect certain individuals with compromised immune systems.”Influenza research is one of the most competitive and difficult arenas in which to secure funding,” said J. Donald Capra, […]
The Oklahoma Medical Research Foundation has welcomed its 50th class of Sir Alexander Fleming Scholars. The class, 13 in all, represent some of Oklahoma’s most talented high school and college science students. The eight high-schoolers and five collegians were selected from more than 100 applicants. the students, all of whom are contemplating careers in medical […]
The University of Oklahoma’s Phi Delta Alpha sorority has presented the Oklahoma Medical Research Foundation with a check to support lupus research at OMRF. This represents the second straight year that Phi Delta Alpha, Oklahoma’s first and only Asian sorority, has made a donation to support lupus research at OMRF. “The members of Phi Delta […]
The Oklahoma Medical Research Foundation has received a $13.8 million grant from the National Institutes of Health to study the toxin that causes anthrax. The grant will pay $2.76 million a year through 2009 and is the largest ever awarded to an Oklahoma institution to fund bioterrorism research.With this grant, nine scientists will explore natural […]
At its semiannual board meeting this evening, the Oklahoma Medical Research Foundation will add Oklahoma First Lady Kim Henry and four others to its board of directors. Joining Henry as new board members will be Gary Pierson, Dave Lopez and Jerome Holmes of Oklahoma City and Gregory Walton, M.D., of Enid. Also this evening, OMRF […]
In a study published tomorrow in The New England Journal of Medicine, scientists report that in patients suffering from systemic lupus erythematosus (commonly known as lupus), autoantibodies – proteins that the body mistakenly unleashes against its own tissue – are typically present years before patients are diagnosed with the disease. This research by scientists at […]
For the second time in 13 months, a substantial gift from the Kerr Foundation has created a new endowed chair at the Oklahoma Medical Research Foundation. The most recent donation will establish the Lou C. Kerr Endowed Chair in Biomedical Research. Robert S. Kerr Jr. made the gift on behalf of the Kerr Foundation in […]
For the second time in 13 months, a substantial gift from the Kerr Foundation has created a new endowed chair at the Oklahoma Medical Research Foundation. The most recent donation will establish the Lou C. Kerr Endowed Chair in Biomedical Research. Robert S. Kerr Jr. made the gift on behalf of the Kerr Foundation in […]
Oklahoma City, OK – The Oklahoma Medical Research Foundation hosted the first international Lupus genetics conference on September 8-9. Although scientists have been using modern approaches to study the genetics of Lupus for the past ten years, there has never been a formal meeting dedicated to the subject. This meeting was meant to facilitate meetings […]
(OKLAHOMA CITY) — Federal judges met to discuss DNA technology today, but instead of wearing their traditional black robes, these judges donned white lab coats. The judges participated in the Oklahoma Medical Research Foundation’s workshop called “Forensic Genetics: A Laboratory Course in Molecular Fingerprinting,” which is a hands-on seminar in DNA technology. This is the […]
Scientists at the Oklahoma Medical Research Foundation have garnered an unprecedented $12.1 million in National Institutes of Health (NIH) grants in 1999, Foundation officials announced today. In a typical year, OMRF receives $7.7 to $8.0 million in competitive grants from NIH. This year, however, the figure shot up by more than 50 percent. While the […]
“From Bench to Bedside: Biomedicine at the New Millennium,” a series of free public lectures presented by scientists at the Oklahoma Medical Research Foundation, is scheduled to begin October 7 at Westminster Presbyterian Church in Oklahoma City. OMRF’s nationally and internationally recognized biomedical researchers will explain in easily understood terms the latest research being done […]
A group of scientists from the Oklahoma Medical Research Foundation (OMRF) today announced that Systemic Lupus Erythematosus (lupus) may be caused by a common virus. Their results will be published today in the The Journal of Clinical Investigation. The work being reported raises suspicion that a common virus, known as Epstein-Barr virus, may be the culprit […]

Under his leadership, OMRF has enjoyed a decade of scientific achievement and historic campus expansion. Still, if you ask Dr. Stephen Prescott, he’ll tell you he’s just getting started. For Dr. Stephen Prescott there was no aha! moment. No instant where everything crystallized and he just knew he had to take the helm of […]