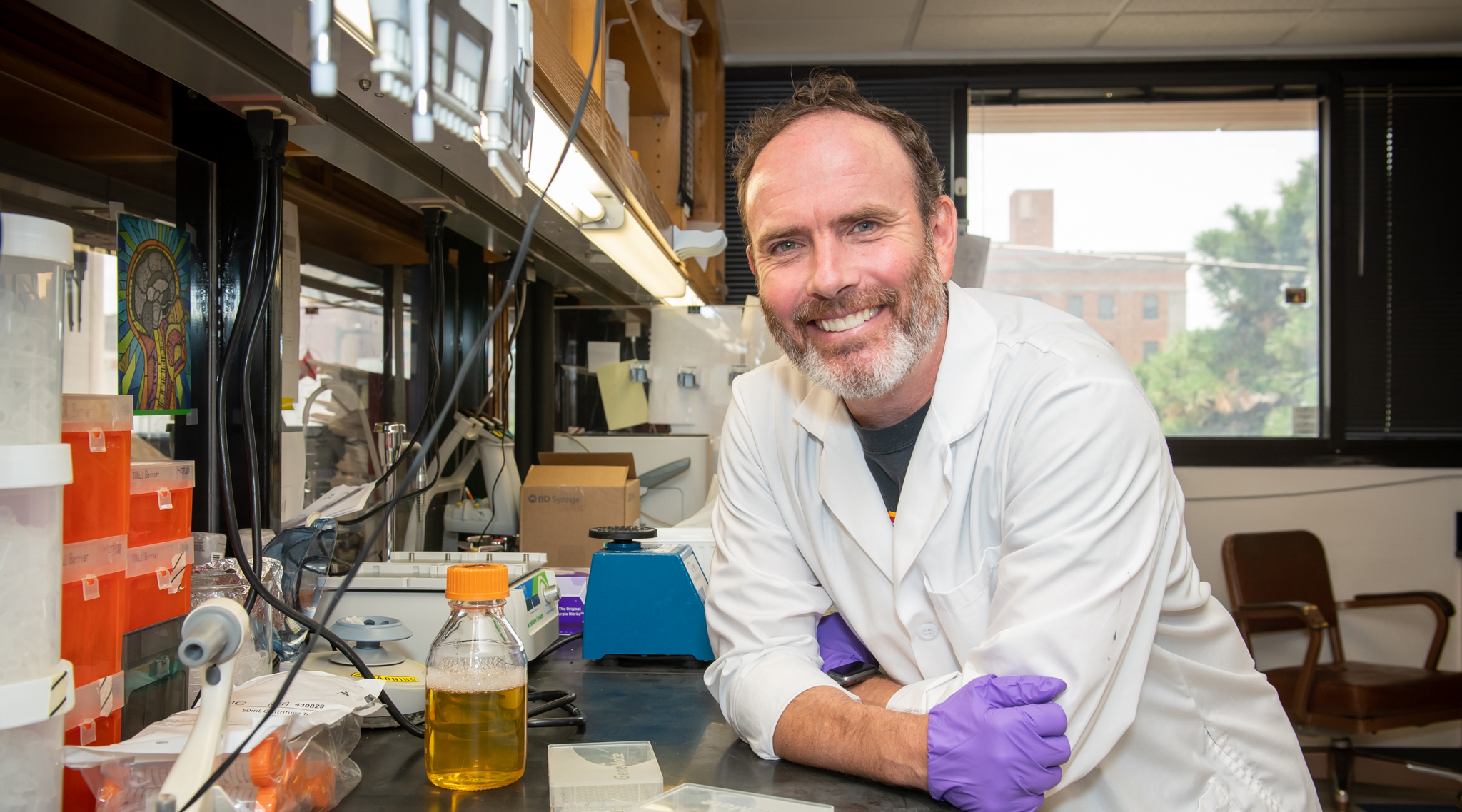
Robert Axtell, Ph.D.
Associate Professor
Arthritis & Clinical Immunology Research Program
My 101
Multiple sclerosis, or MS, is an autoimmune disease that affects the ability of the nervous system to carry signals to and from the brain. Inflammation causes damage to myelin, the protective covering that surrounds nerve cells, slowing and sometimes blocking nerve impulses. The disease carries with it a variety of symptoms, including problems with vision, tremors, paralysis, painful spasms, imbalance, and cognitive changes.
While MS shares some similarities with lupus, Sjögren’s Syndrome, and other autoimmune diseases, it actually is the “black sheep” of autoimmune diseases. Drugs that are used to treat rheumatoid arthritis and lupus actually make MS worse and vice versa.
In my lab, we use animal models and patient samples from OMRF’s MS Center of Excellence to understand why MS behaves differently from other autoimmune diseases and why some MS patients do not respond well to standard therapy. By studying human disease specimens and animal models, we have great potential to identify new therapeutic targets and develop prognostic tests that will bring clinical care of multiple sclerosis into the forefront of personalized medicine.
Research
Multiple sclerosis (MS) is a highly heterogeneous disease with significant variability in the clinical course to the pathological patterns observed in brain lesions. Clinically, the heterogeneity in MS is illuminated by the variability in response to interferon-β (IFN-β) therapy. Even though there are clear responders and non-responders to IFN-β, there are limited tools to predict and monitor responsiveness to this therapy. My laboratory has utilized both clinical samples from MS patients and animal models of MS to identify the biological pathways that impact response to IFN-β therapy. These studies have uncovered key biological mechanisms that are specific to IFN-β therapy and, furthermore, they have shed light on general immunological processes of MS and neuro-inflammation.
Research Highlights:
- Immunological heterogeneity impacts treatment response to IFN-β in patients with MS.
I recently led a collaboration, which assessed serum cytokines for their utility to predict and monitor response to IFN-β therapy in a large cohort of MS patients (Hegen et al. Neurol Neuroimmunol Neuroinflamm. 2016). We found that specific cytokine profiles could separate MS into six distinct subgroups that have differential clinical response to therapy. Two subsets, which had similar but distinct TH17 signatures, were associated with poor response to IFN-β therapy. Two other immunologically distinct subsets were associated with good response to therapy. These data suggest that the MS population has immunologically distinct subgroups that can stratify treatment response to IFN-β. Moreover, these data provide strong evidence that serum cytokines can be informative biomarkers for monitoring disease in MS patients.
- The T Helper (TH) 17 pathway dictates non-response to IFN-β therapy in mice with EAE.
Neuro-autoimmune disorders can be initiated by two different T-cell subtypes: TH1 and TH17 cells. Using the experimental autoimmune encephalomyelitis (EAE) mouse model of MS, I discovered that the response to IFN-β is dictated by whether the disease is TH1 or TH17 driven (Axtell et al. Nat Med. 2010). IFN-β treatment reduced disease in mice with TH1-driven EAE, and conversely, IFN-β treatment exacerbated disease in mice with TH17-driven EAE. These animal data are congruent with our studies of serum samples from MS patients (described above) and further supports that the EAE model has clinical relevance for MS.
- Regulatory B-cells play a key role in the efficacy of IFN-β in both patients with MS and mice with EAE.
We published that MS patients successfully treated with IFN-β had significant increases in BAFF (a cytokine that supports B-cell development and function) and a skewing in the B-cell population away from inflammatory B-cells and toward anti-inflammatory B-cells. Similarly, in mice with TH1-EAE, effective IFN-β treatment increased serum BAFF levels and numbers of regulatory B-cells. Furthermore, mice deficient in B-cells do not benefit from IFN-β treatment (Schubert et al. J Immunol. 2015). These data show that IFN-β therapy requires immune regulation via B-cells to effectively reduce TH1-mediated neuro-inflammation in both EAE and MS.These results may also explain the failure of the large clinical trial of Atacicept for relapsing remitting MS. Atacicept (a BAFF blocker) increased relapse rates in MS and we speculate that this treatment suppressed the same B-cell regulatory activity required for IFN-β efficacy.
Impact of Our Research
Our research has shown that specific immune pathways driving neuro-inflammation have clinically significant consequences. We demonstrated that disease phenotypes with elevated TH17/neutrophil signatures, unlike Th1 driven disease, do not respond well to conventional MS therapies. Clinically, these include highly inflamed relapsing remitting MS, neuromyelitis optica (NMO), and progressive MS (data from Dr. Segal at the University of Michigan). Currently, there is a lack of effective treatment options for progressive MS and NMO. Therefore, further characterization of these diseases will provide insights into novel treatment strategies for these underserved patients.
Our observations from human and mouse studies suggest the following biological paradigm. Neuro-autoimmune patients who do not respond to conventional therapies have a strong auto-reactive TH17 response that initiates the recruitment of neutrophils and other inflammatory myeloid cells into the CNS where they support the proliferation of inflammatory B-cells. In contrast, patients who are effectively managed with conventional therapies have a TH1-predominant disease where B-cells have a regulatory response. My studies have addressed three key issues in the field of MS/neuro-inflammation.
- The biological heterogeneity in the MS population impacts the prognosis of this disease. Our studies have identified a series of serum-based biomarkers that could have prognostic utility in MS.
- The balance of inflammatory and regulatory B-cells are key in modulating disease activity in MS. Considering that therapies specifically targeting B-cells are emerging for MS, our studies on B-cells populations are highly relevant and could impact how patients are monitored while on B-cell depleting therapies.
- Our studies have described an underappreciated role of BAFF in TH1- and TH17- induced inflammation, which has provided a plausible explanation for the failure of Atacicept in MS.
Brief CV
Education
B.S., Idaho State University, Pocatello, ID, 1999
M.S., Idaho State University, Pocatello, ID, 2001
Ph.D., University of Alabama at Birmingham, 2007
Postdoc, Stanford University, 2007-2013
Honors and Awards
2003 UAB Microbiology Retreat: Outstanding Oral Presentation Award
2004 UAB Medicine Trainee Research Symposium: 1st place graduate student poster
2005 UAB Graduate Research Day symposium: 1st place oral presentation
2007 UAB Department of Microbiology: Outstanding Student Award
2007 UAB Joint Health Sciences: Outstanding Student Award
2010 Stanford Cancer and Immunology Postdoc Symposium: 1st Place Oral Presentation
2010 The Whitaker Prize for MS Research. The Consortium of Multiple Sclerosis Centers
2010 Stanford Program of Immunology: Post Doctoral Mentor of the Year
2011 European Committee for Treatment and Research in Multiple Sclerosis: 3rd place - Young Scientist Poster Presentation
2016 OMRF Fred Jones Award for Scientific Achievement
Professional Activities
Grant reviews: Ad hoc Reviewer: Natural Sciences and Engineering Research Council of Canada, National Institutes of Health – Small Business, Innovative Immunology Research, Canadian Institutes of Health Research; Reviewer: National Multiple Sclerosis Society – Pilot Grants, National Multiple Sclerosis Society – Research Grants
Journal Reviews (in alphabetical order): Acta Neuropathologica, Annals of Clinical and Translational Neurology, Frontiers in Immunology, Immunology and Cell Biology, International Immunology, Neuroscience
Educational Activities: Mentoring of students: PhD Candidates, GPiBs rotating graduate students, OMRF Fleming Scholars Summer Research Program
Institutional Committees: OMRF IACUC Committee Member, Fleming Scholar Admissions Committee, OUHSC PhD Thesis Committees
Memberships
American Association of Immunologists
International Society for Interferon and Cytokine Research
American Academy of Neurology
Joined OMRF scientific staff in 2013
Publications
Recent Publications
Allushi B, Chlebicz M, Kumar G, Massey K, Labombarde JG, Turner S, Miller RAJ, Williams AP, Quinn A, Kovats S, Axtell RC. Interferon-β treatment reverses the detrimental effect of B-cell depletion therapy on respiratory virus infection. J Immunol, 2025 May, PMID: 40334083
Reidy M, Khan M, Mills EA, Wu Q, Garton J, Draayer DE, Zahoor I, Giri S, Axtell RC, Mao-Draayer Y. New Frontiers in Multiple Sclerosis Treatment: From Targeting Costimulatory Molecules to Bispecific Antibodies. Int J Mol Sci 26, 2025 April, PMID: 40332536, PMCID: PMC12028294
Cordeiro B, Ahn JJ, Gawde S, Ucciferri C, Alvarez-Sanchez N, Revelo XS, Stickle N, Massey K, Brooks DG, Guthridge JM, Pardo G, Winer DA, Axtell RC, Dunn SE. Obesity intensifies sex-specific interferon signaling to selectively worsen central nervous system autoimmunity in females. Cell Metab, 2024 August, PMID: 39168127, PMCID: PMC11463735
Selected Publications
Hegen H, Millonig A, Bertolotto A, Comabella M, Giovanonni G, Guger M, Hoelzl M, Khalil H, Killestein J, Lindberg R, Malucchi S, Mehling M, Montalban X Polman CHm Rudzki D, Schautzer F, Sellebjerg F, Sorensen PS, Deisenhammer F, Steinman L, Axtell RC. Cytokine profiles demonstrate heterogeneity of Interferon-beta response in patients with multiple sclerosis. Neurol Neuroimmunol Neuroinflamm. 2016 Jan 27;3(2):e202. eCollection 2016 Apr. PMID: 26894205, PMCID: PMC4747480
Quinn JL, Kumar G, Agasing A, Ko R, Axtell RC. Role of TFH Cells in Promoting T Helper 17-Induced Neuro-inflammation. Front Immunol. 2018 Feb 27;9:382. eCollection 2018. PMID: 29535739, PMCID: PMC5835081
Agasing AM, Wu Q, Khatri B, Borisow N, Ruprecht K, Brandt AU, Gawde S, Kumar G, Quinn JL, Ko RM, Mao-Draayer Y, Lessard CJ, Paul F, Axtell RC. Transcriptomics and proteomics reveal a cooperation between interferon and T-helper 17 cells in neuromyelitis optica. Nat Commun. 2020 Jun 5;11(1):2856. PMID: 32503977, PMCID: PMC7275086
Towner RA, Smith N, Zalles M, Morris S, Toliver M, Saunders D, Lerner M, Kumar G, Axtell RC. ELTD1 as a biomarker for multiple sclerosis: Pre-clinical molecular-targeted studies in a mouse experimental autoimmune encephalomyelitis model. Mult Scler Relat Disord. 2021 Apr;49:102786. doi: 10.1016/j.msard.2021.102786. Epub 2021 Jan 22. PMID: 33517175, PMCID: PMC8068591 (available on 2022-04-01)
Kumar G, Maria Z, Kohli U, Agasing A, Quinn JL, Ko RM, Zamvil SS, Axtell RC. CNS-autoimmune responses in BCMA-deficient mice provide insight for the failure of atacicept in MS. Neurol Neuroimmunol Neuroinflamm. 2021 Mar 1;8(3):e973. doi: 10.1212/NXI.0000000000000973. Print 2021 May. PMID: 33649164, PMCID: PMC7954465
Holloman JP, Axtell RC, Monson NL, Wu GF. The Role of B Cells in Primary Progressive Multiple Sclerosis. Front Neurol. 2021 Jun 7;12:680581. doi: 10.3389/fneur.2021.680581. eCollection 2021. PMID: 34163430, PMCID: PMC8215437.
Contact
Arthritis & Immunology Research Program, MS 24
Oklahoma Medical Research Foundation
825 N.E. 13th Street
Oklahoma City, OK 73104
Phone: (405) 271-2354
Fax: (405) 271-4110
E-mail: bob-axtell@omrf.org
For media inquiries, please contact OMRF’s Office of Public Affairs at news@omrf.org.
Lab Staff
Rose Ko, Ph.D.
Associate Staff Scientist
Gaurav Kumar, Ph.D.
Assistant Staff Scientist
Kaylea Massey
Research Technician
Bujana Allushi
Graduate Student
Emma Newton
Graduate Student
Melissa Testut
Graduate Student
Louise Williamson
Finance and Administrative Specialist