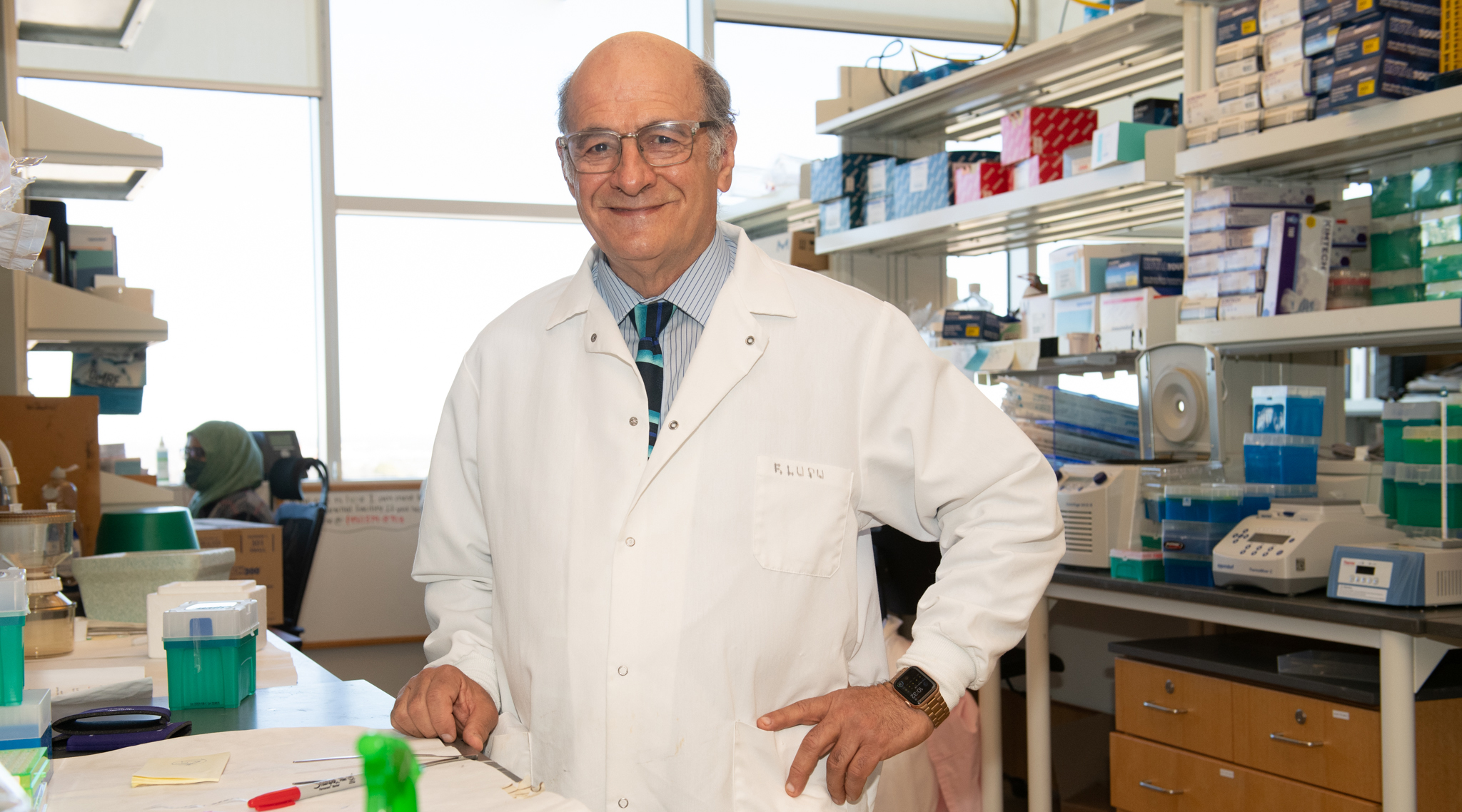
Florea Lupu, Ph.D.
Professor
Cardiovascular Biology Research Program
H. Allen & Mary K. Chapman Chair in Medical Research
Adjunct Professor, Department of Pathology, Department of Cell Biology, Department of Medicine, University of Oklahoma Health Sciences Center
My 101
Blood clotting plays an important role in the body. We depend on clotting to help close wounds and keep us from bleeding too much. But when we clot more than normal, it can lead to heart attack, stroke, or other diseases of the cardiovascular system.
We look not only at blood itself but also at the way it interacts with the inside lining of the blood vessels, called the endothelium. This thin layer of cells works with the blood, so the latter knows when to clot—or not. In particular, we study the process that controls the start of blood clotting at the point where the blood and the vessel wall interact.
We also study the changes that lead to the formation of unwanted and/or excessive blood clots during sepsis. Sepsis is a serious blood infection that kills approximately 11 million people worldwide each year. It occurs when the body must fight a severe infection that has spread through the body via the bloodstream. If a patient develops sepsis, they will likely suffer widespread blood clotting coupled with a state of low blood pressure called “shock.” This condition can develop either because of the body’s own defense system or from toxic substances made by infectious agents, such as bacteria and viruses, like the SARS-CoV-2 that causes the potentially deadly COVID-19.
Research
The main focus of our work is directed to the pathophysiology and therapy of sepsis. In particular we look at the steps involved in the progression of sepsis and how they lead to organ damage and, many times, death. Our group studies bacterial sepsis that occurs from exposure to Escherichia coli, Staphylococcus aureus or anthrax and the sequence of overlapping disease conditions involved, any one of which can be lethal. Furthermore, we are testing new therapies targeting the contact phase pathways that initiate blood clotting, and the complement activation mechanisms and immune responses associated with these pathways. Both lines of investigation aim to provide in-depth knowledge on potentially new drugs that will prevent organ damage and death in septic patients. A new research project is directed toward the identification of biomarkers that can predict the stage and the outcome of sepsis and can help the physician apply the most appropriate treatment. By learning more about the way sepsis infection develops and spreads, we hope to find ways to diagnose the condition earlier and develop more effective ways to treat it.
Another line of research focuses on what triggers the normal blood clotting system. We study a protein on the surface of vascular cells that is responsible for telling the blood to clot. This protein, known as tissue factor, is strictly regulated by a natural inhibitor called tissue factor pathway inhibitor (TFPI). We also discovered a novel protein called ADTRP that could play a role in the modulation of TFPI function. By looking at the ways that TFPI is regulated in the vessels, we hope to identify new proteins involved in the process and increase our understanding of blood clotting.
Brief CV
Education
M.S., Faculty of Biology, University of Cluj, Romania, 1975
Ph.D., Institute of Cellular Biology and Pathology, Bucharest, Romania, 1986
Honors and Awards
1983 Fulbright Fellow, US Council for International Exchange of Scholars
1994 Young Investigator Award of American Health Association
2018 H. Allen & Mary K. Chapman Chair in Medical Research, Oklahoma Medical Research Foundation
Other Activities
Serves as Associate Editor of the Journal of Cellular and Molecular Medicine.
Reviews articles submitted to Blood, Blood Advances, Proceedings of National Academy of Sciences of U.S.A., Journal of Cell Biology, Journal of Biological Chemistry, Journal of Cellular and Molecular Medicine, Circulation, Circulation Research, Journal of Thrombosis and Haemostasis, Thrombosis and Haemostasis, Arteriosclerosis Thrombosis and Vascular Biology, Haemostasis, etc.
Reviews grants submitted to National Institutes of Health, American Heart Association, British Heart Foundation, Science Foundation of Ireland, Wellcome Trust, Austrian National Science Foundation, and European Union.
Memberships
Romanian Society for Cell Biology, 1982
European Vascular Biology Organization, 1986
International Society for Haemostasis and Thrombosis, 1991
International Society for Fibrinolysis and Thrombolysis, 1992
Royal Microscopical Society, 1994
European Immunocytochemistry Club, 1994
American Society of Hematology, 2002
American Society for Investigative Pathology, 2003
Histochemical Society, 2003
American Thoracic Society, 2011
American Association of Immunologists, 2013
American Heart Association, 2013
Joined OMRF scientific staff in 2001
Publications
Recent Publications
Geng X, Chen L, Ahmed Z, Formigari GP, Ho YC, Del Gaudio I, Datilo MN, Azartash-Namin ZJ, Heron C, Shan X, Keshari RS, Pal S, Chen H, Lupu F, Xia L, Randolph GJ, Zawieja SD, Camerer E, Davis MJ, Srinivasan RS. S1PR1 regulates lymphatic valve development and tertiary lymphoid organ formation in the ileum. J Exp Med 222, 2025 September, PMID: 40553105, PMCID: PMC12187108
Silasi R, Keshari RS, Abe T, Byrum SD, Regmi G, Lupu C, Georgescu C, Simmons JH, Shamanaev A, Moellmer SA, Puy C, Shatzel JJ, Province D, Edmondson RD, Mackintosh SG, Avaritt NL, Bloomfield D, Gailani D, Tackett AJ, McCarty OJT, Lupu F. Protective Effects of FXI Inhibition by Abelacimab in a Baboon Model of Live Staphylococcus aureus Sepsis. J Thromb Haemost, 2025 June, PMID: 40582699
Lira AL, Taskin B, Puy C, Keshari RS, Silasi R, Pang J, Aslan JE, Shatzel JJ, Lorentz CU, Tucker EI, Schmaier AH, Gailani D, Lupu F, McCarty OJT. The physicochemical properties of lipopolysaccharide chemotypes regulate activation of the contact pathway of blood coagulation. J Biol Chem:108110, 2024 December, PMID: 39706265, PMCID: PMC11773025
Selected Publications
Silasi R, Keshari RS, Regmi G, Lupu C, Georgescu C, Simmons JH, Wallisch M, Kohs TCL, Shatzel JJ, Olson SR, Lorentz CU, Puy C, Tucker EI, Gailani D, Strickland S, Gruber A, McCarty OJT, Lupu F. Factor XII plays a pathogenic role in organ failure and death in baboons challenged with Staphylococcus aureus. Blood. 2021 Jul 15;138(2):178-189. doi: 10.1182/blood.2020009345. PMID: 33598692; PMCID: PMC8288658.
Keshari RS, Silasi R, Popescu NI, Georgescu C, Chaaban H, Lupu C, McCarty OJT, Esmon CT, Lupu F. Fondaparinux pentasaccharide reduces sepsis coagulopathy and promotes survival in the baboon model of Escherichia coli sepsis. J Thromb Haemost. 2020 Jan;18(1):180-190. doi: 10.1111/jth.14642. Epub 2019 Oct 16. PMID:31549765; PMCID: PMC6940562.
Silasi R, Keshari RS, Lupu C, Van Rensburg WJ, Chaaban H, Regmi G, Shamanaev A, Shatzel JJ, Puy C, Lorentz CU, Tucker EI, Gailani D, Gruber A, McCarty OJT, Lupu F. Inhibition of contact-mediated activation of factor XI protects baboons against S aureus-induced organ damage and death. Blood Adv. 2019 Feb 26;3(4):658-669. doi: 10.1182/bloodadvances.2018029983. Erratum in: Blood Adv. 2020 Aug 11;4(15):3741. PMID: 30808684; PMCID: PMC6391670.
Popescu NI, Silasi R, Keshari RS, Girton A, Burgett T, Zeerleder SS, Gailani D, Gruber A, Lupu F, Coggeshall KM. Peptidoglycan induces disseminated intravascular coagulation in baboons through activation of both coagulation pathways. Blood. 2018 Aug 23;132(8):849-860. doi: 10.1182/blood-2017-10-813618. Epub 2018 Jun 19. PMID: 29921614; PMCID: PMC6107880.
Keshari RS, Silasi R, Lupu C, Taylor FB Jr, Lupu F. In vivo-generated thrombin and plasmin do not activate the complement system in baboons. Blood. 2017 Dec 14;130(24):2678-2681. doi: 10.1182/blood-2017-06-788216. Epub 2017 Oct 11. PMID: 29021229; PMCID: PMC5731087.
Keshari RS, Silasi R, Popescu NI, Patel MM, Chaaban H, Lupu C, Coggeshall KM, Mollnes TE, DeMarco SJ, Lupu F. Inhibition of complement C5 protects against organ failure and reduces mortality in a baboon model of Escherichia coli sepsis. Proc Natl Acad Sci U S A. 2017 Aug 1;114(31):E6390-E6399. doi:10.1073/pnas.1706818114. Epub 2017 Jul 18. PMID: 28720697; PMCID: PMC5547645.
Contact
Cardiovascular Biology Research Program, MS 45
Oklahoma Medical Research Foundation
825 N.E. 13th Street
Oklahoma City, OK 73104
Phone: (405) 271-7462
Fax: (405) 271-7417
E-mail: Florea-Lupu@omrf.org
For media inquiries, please contact OMRF’s Office of Public Affairs at news@omrf.org.
Lab Staff
Robert Silasi-Mansat, Ph.D.
Research Assistant Professor
Cristina Lupu, Ph.D.
Staff Scientist
Ravi Keshari, Ph.D.
Associate Staff Scientist
Vivian Taylor
Research Technician I
Mia Pederson-Rambo
Project Coordinator I
News from the Lupu lab
The Oklahoma Medical Research Foundation announced today that it has received a $10 million grant from the National Institutes of Health. “This is yet another important step in the emergence of Oklahoma as a center of biomedical excellence,” said OMRF President Dr. J. Donald Capra. “Five years ago, this state had never seen a $10 […]