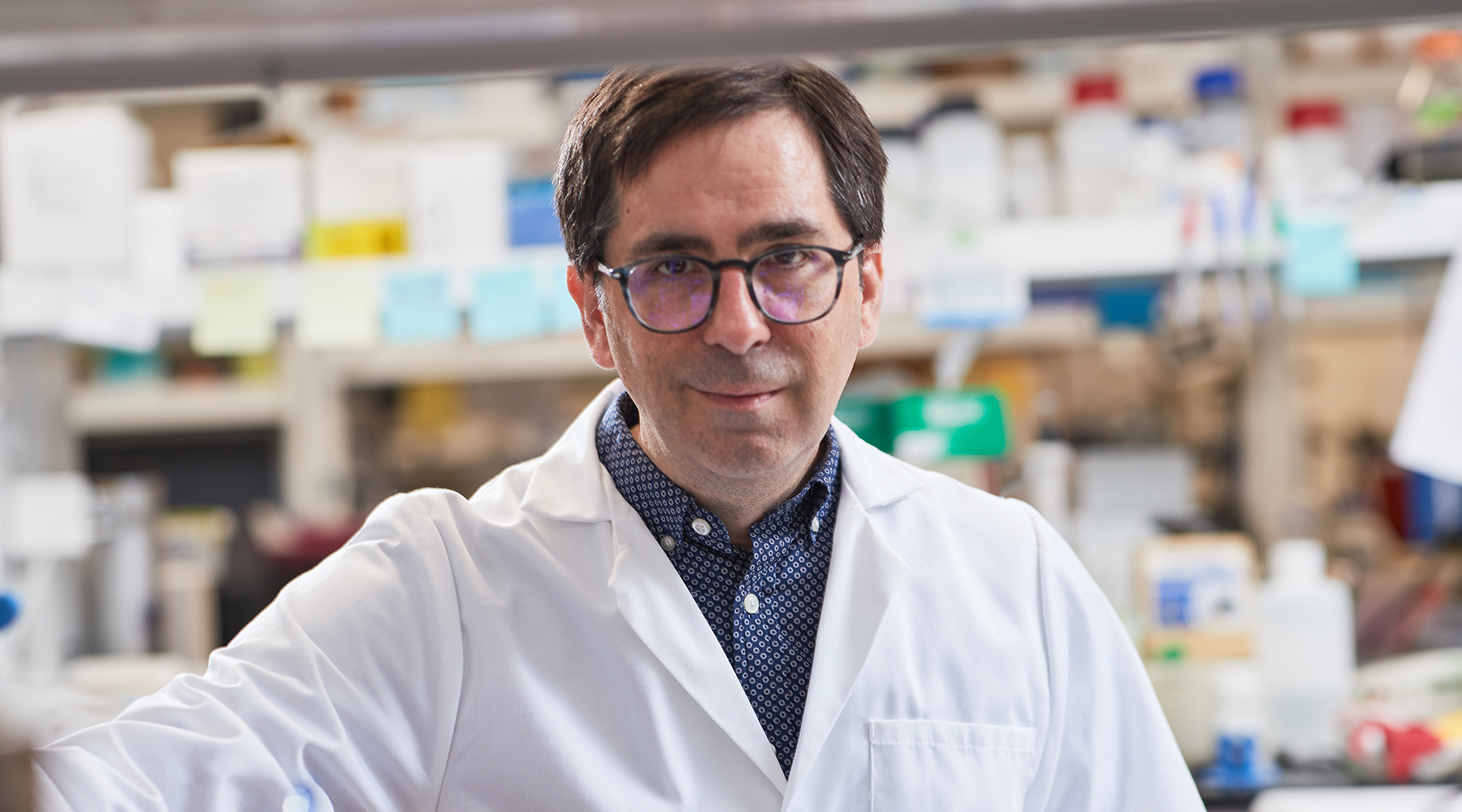
Kenneth M. Humphries, Ph.D.
Associate Professor
Aging & Metabolism Research Program
Adjunct Assistant Professor, Department of Geriatric Medicine, Geroscience and Healthy Brain Aging, and Department of Biochemistry and Molecular Biology, University of Oklahoma Health Sciences Center
My 101
Diabetes is a worldwide epidemic that causes a multitude of health problems. My laboratory is primarily interested in how diabetes affects the heart. This is an important area of research because diabetes increases both the occurrence and progression of heart disease and heart failure. Our goal is to better understand the underlying causes so that better treatment options can be developed to prevent and treat diabetic heart disease.
The heart never fatigues and has an unyielding need for energy. In healthy people, the heart derives this energy primarily from lipids (fats) and glucose (sugar). This is problematic in people with types 1 and type 2 diabetes because sugar is not used properly used by the heart. This is because insulin, which causes cells in the heart to use sugar, is not made in sufficient quantities and/or because insulin no longer works properly. The consequence is that the circulating sugar levels are increased, but paradoxically it is unavailable to be burned in muscles such as the heart.
Our research focuses on two aspects of how diabetes affects the heart. First, we are examining how mitochondria, the parts of the cell that convert nutrients into energy, are affected by diabetes. Changes in mitochondria further prevent the heart from using glucose properly. Furthermore, damage to these organelles impedes cardiac energy production and creates toxic free radicals. The second area of research is examining how the molecular switches that normally allow the heart to use glucose get stuck in the “off” position. The ultimate goals of these studies are to find ways to prevent or reverse diabetic heart disease.
Research
The research in my laboratory is focused on understanding how diabetes affects the heart so that better treatment options can be developed. This is especially important given the high incidence of diabetes and ensuing cardiovascular complications. Indeed, diabetes induces changes to cardiac function in the absence of other risk factors through mechanisms that are not completely clear.
One of our projects is examining how the beta-adrenergic signaling pathway is affected by diabetes, and how these changes may exacerbate and enhance stress on the heart. Activation of cAMP-dependent protein kinase (PKA) via beta-adrenergic receptor signaling is a primary means of increasing cardiac contractility. Over-activation or dysregulation of this pathway is a major driver of diabetic cardiomyopathy, life threatening arrhythmias, and heart failure. However, the mechanisms by which this pathway becomes disrupted are largely unknown. In the healthy heart, PKA increases contractility by amplifying calcium cycling and concertedly activating phosphofructose kinase-2 (PFK-2) to promote glucose oxidation. In this manner, workload and metabolic demand are finely orchestrated. We have identified important changes in both PKA signaling and PFK-2 activation that may drive diabetic cardiomyopathy. Ongoing studies are determining the molecular mechanisms of this signaling dysfunction to identify potential points of intervention.
The second project in our lab is examining how mitochondrial function is affected by diabetes. The heart’s constant demand for energy is primarily derived from fatty acids and secondarily from glucose. Diabetes leads to metabolic inflexibility, in which the capacity of the heart to use glucose is greatly diminished. While changes in glucose metabolism occur in the cytoplasm, we have shown that there are alterations in mitochondrial function that further promote metabolic flexibility. This may be an important determinant in the occurrence or progression of diabetic cardiomyopathy. We have shown that these changes in mitochondrial function are mediated, in part, by overabundance of acetylated proteins. We are working to understand how hyper-acetylation occurs, how it affects mitochondrial function, and how it can be alleviated. There are currently no therapeutics that specifically target mitochondrial abnormalities and diabetic cardiomyopathy. The results of this research will determine if preventing or reversing mitochondrial acetylation is a promising target for therapeutic intervention.
Brief CV
Education
B.S., John Carroll University, University Heights, OH, magna cum laude, 1995
Ph.D., Case Western Reserve University, Cleveland, OH, 2000
Postdoctoral Fellow, Howard Hughes Medical Institute, University of California, San Diego, CA, 2000-2005
Honors and Awards
President’s and American Values Scholarships, John Carroll University, 1991-1995
American Chemical Society Award in Quantitative Analysis, 1994
Alpha Sigma Nu National Honor Society, John Carroll University, 1994
NIH Institutional Predoctoral Fellowship (T32 HL07653), 1996-1998
NIH Institutional Postdoctoral Fellowship (T32 CA009523), 2000-2001
NIH Individual Postdoctoral Fellowship (F32 GM64991), 2001-2003
Fred Jones Award for Scientific Achievement, OMRF, 2019
Memberships
American Association for the Advancement of Science
American Chemical Society
American Diabetes Association
American Heart Association
Joined OMRF scientific staff in 2006
Publications
Recent Publications
Szulta A, Wang L, Hasan A, Kinter M, Pranay A, Zhu J, Humphries KM, Loveland B, Griffin TM, Bieniasz M. The Identification of a Key Regulator of Mitochondrial Metabolism, the LRPPRC Protein, as a Novel Therapeutic Target in SDHA-Overexpressing Ovarian Tumors. Cancers (Basel) 17, 2025 June, PMID: 40563592, PMCID: PMC12190274
Eeda V, Hedrick AF, Pranay A, Humphries KM, Heidenreich E, Awasthi V. Cardiotropic ligand-guided liposomes for myocardial delivery of atorvastatin in a mouse model of myocardial infarction. Int J Pharm 681:125841, 2025 June, PMID: 40499599
Harold KM, Matsuzaki S, Pranay A, Zhu J, Faakye A, Humphries KM. PFKFB2 is Pivotal for Metabolic Flexibility and Differential Glucose Utilization. bioRxiv, 2025 May, PMID: 40502119, PMCID: PMC12154713
Selected Publications
Harold KM, Matsuzaki S, Pranay A, Loveland BL, Batushansky A, Mendez Garcia MF, Eyster C, Stavrakis S, Chiao YA, Kinter M, Humphries KM. Loss of Cardiac PFKFB2 Drives Metabolic, Functional, and Electrophysiological Remodeling in the Heart. J Am Heart Assoc. 2024 Apr 2;13(7):e033676. doi: 10.1161/JAHA.123.033676. Epub 2024 Mar 27. PMID: 38533937; PMCID: PMC11179765.
Mendez Garcia MF, Matsuzaki S, Batushansky A, Newhardt R, Kinter C, Jin Y, Mann SN, Stout MB, Gu H, Chiao YA, Kinter M, Humphries KM. Increased cardiac PFK-2 protects against high-fat diet-induced cardiomyopathy and mediates beneficial systemic metabolic effects. iScience. 2023 Jun 15;26(7):107131. doi: 10.1016/j.isci.2023.107131. PMID: 37534142; PMCID: PMC10391959.
Matsuzaki S, Eyster C, Newhardt MF, Giorgione JR, Kinter C, Young ZT, Kinter M, Humphries KM. Insulin signaling alters antioxidant capacity in the diabetic heart. Redox Biol. 2021 Nov;47:102140. doi: 10.1016/j.redox.2021.102140. Epub 2021 Sep 20. PMID: 34560411; PMCID: PMC8473541.
Newhardt MF, Batushansky A, Matsuzaki S, Young ZT, West M, Chin NC, Szweda LI, Kinter M, Humphries KM. Enhancing cardiac glycolysis causes an increase in PDK4 content in response to short-term high-fat diet. J Biol Chem. 2019 Nov 8;294(45):16831-16845. doi: 10.1074/jbc.RA119.010371. Epub 2019 Sep 27. PMID: 31562244; PMCID: PMC6851294.
Batushansky A, Matsuzaki S, Newhardt MF, West MS, Griffin TM, Humphries KM. GC-MS metabolic profiling reveals fructose-2,6-bisphosphate regulates branched chain amino acid metabolism in the heart during fasting. Metabolomics. 2019 Jan 28;15(2):18. doi: 10.1007/s11306-019-1478-5. PMID: 30830475; PMCID: PMC6478396.
Bockus LB, Matsuzaki S, Vadvalkar SS, Young ZT, Giorgione JR, Newhardt MF, Kinter M, Humphries KM. Cardiac Insulin Signaling Regulates Glycolysis Through Phosphofructokinase 2 Content and Activity. J Am Heart Assoc. 2017 Dec 4;6(12):e007159. doi: 10.1161/JAHA.117.007159. PMID: 29203581; PMCID: PMC5779029.
Contact
Aging & Metabolism Research Program, MS 46
Oklahoma Medical Research Foundation
825 N.E. 13th Street
Oklahoma City, OK 73104
Phone: (405) 271-7584
Fax: (405) 271-1437
E-mail: Kenneth-Humphries@omrf.org
For media inquiries, please contact OMRF’s Office of Public Affairs at news@omrf.org.
Lab Staff
Satoshi Matsuzaki, Ph.D.
Staff Scientist
Craig Eyster, Ph.D.
Associate Staff Scientist
Jennifer Giorgione, Ph.D.
Associate Staff Scientist
Atul Pranay, Ph.D.
Associate Staff Scientist
Andy Gamez-Rico
Research Technician I
Anna Faakye
Graduate Student
Kylene Harold
Graduate Student
Holly Smith
Administrative Assistant III
News from the Humphries lab
A new wave of researchers has joined the Oklahoma Medical Research Foundation’s scientific staff as part of the foundation’s expansion. OMRF has added seven new scientists to its staff. In addition, two research assistants have been promoted to faculty-level positions. The new researchers have come to OMRF from a variety of institutions across the U.S. […]