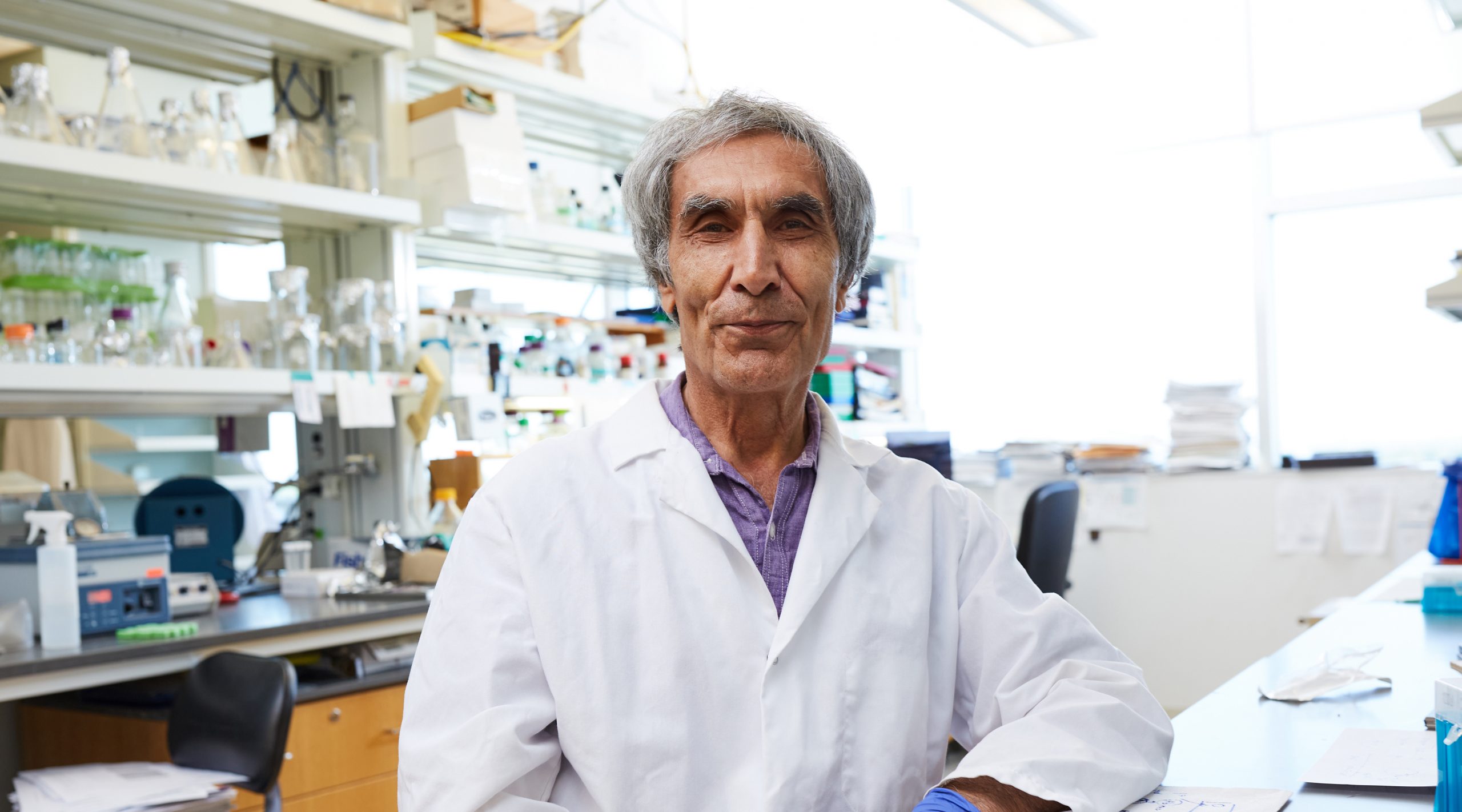
Ray Rezaie, Ph.D.
Professor
Cardiovascular Biology Research Program
My 101
The research in my laboratory is focused on understanding how blood-clotting factors in circulation function together to stop bleeding when a blood vessel is injured. Under normal conditions, clotting factors circulate in blood as inactive molecules. This is because the signal that can trigger the activation of clotting factors is hidden under the cells that line the blood vessels. These cells, called endothelial cells, also have clot-inhibiting receptors on their surfaces to ensure that blood remains in fluid form in the circulation.
When there is an injury to a blood vessel, the hidden signal is now exposed in the vessel system that communicates a wound has occurred. It also signals these inactive molecules to become activated and launch into action. That is when these molecules initiate a cascade that involves numerous other proteins and several chemical reactions that finally end up generating a blood clot. That clot then will seal the site of the wound, which is exactly how it should work.
Upon sealing the wound site, this process needs to stop or it opens up a new set of other problems. The clot generation can become dangerous if it goes unregulated. If the process goes awry, the blood has the potential to make so many clots that it can turn the veins into something like gelatin. That is why it is so critical for it to be localized at the particular site of the wound and produce enough clotting to form a plug, but no more than that. For that to occur, the system has to shut down the clotting action and inactivate all the previously activated proteins once the process is finished. If these are not deactivated, thrombotic problems such as heart attacks and strokes can occur.
My lab studies how these processes work, and by having a better understanding of them, we can develop novel strategies to treat patients.
Research
Coagulation and inflammation are closely linked pathways. Both pathways can be activated when there is an injury to the blood vessel and/or a foreign substance (bacteria or virus) enters circulation. The molecular players in both pathways have extensive interactions in order to full-fill their physiological functions (i.e., stop bleeding and mount inflammatory responses). Thus, in addition to clotting fibrinogen to fibrin clots during coagulation, the proteases of the coagulation cascade also interact with specific vascular cell surface receptors to modulate inflammatory responses. Similarly, inflammatory cytokines secreted during inflammation, not only activate immune cells to fight infection but they also play pivotal roles in regulating coagulation reactions. Two natural anticoagulant pathways, namely protein C and antithrombin (AT) pathways are known to regulate both coagulation and inflammatory reactions. The current focus of our laboratory is on understanding the mechanisms through which these two pathways operate at the molecular level. The protein C pathway is initiated when thrombin binds to endothelial cell surface receptor thrombomodulin (TM) to activate protein C (APC). Several years ago, OMRF investigator, Dr. Charles Esmon, who has discovered TM, also discovered that another receptor called endothelial protein C receptor (EPCR) significantly accelerates the protein C activation reaction. Dr. Esmon’s group found that the N-terminal Gla-domain of both protein C and APC binds EPCR with a similar equilibrium dissociation constant of approximately 30 nM. APC can dissociate from EPCR and form a complex with the vitamin K-dependent cofactor, protein S, to rapidly degrade cofactors Va and VIIIa on negatively charged phospholipids that have become exposed on injured cells and/or activated platelets. Interestingly, when APC remains associated with EPCR, the resulting protease-receptor complex activates the G-protein coupled receptor, protease-activated receptor 1 (PAR1), thereby eliciting physiologically significant cytoprotective and antiinflammatory responses in the vasculature. This finding was initially controversial since thrombin can activate PAR1 with an efficiency that is greater than three orders of magnitude higher than that of APC and that the activation of PAR1 by thrombin initiates potent proinflammatory responses in endothelial cells. During the last few years, our laboratory has developed innovative approaches to investigate these apparent PAR1-depependent paradoxical signaling responses by APC and thrombin. We have discovered that all three receptors involved (TM, EPCR and PAR1) in protein C activation and signaling are co-localized within caveolin-1 containing membrane lipid-rafts of endothelial cells and that when EPCR is occupied by either protein C or APC, the activation of PAR1 by either APC or thrombin is cytoprotective independent of the protease activating PAR1. Our results have indicated that the ligand occupancy and association of receptors with caveolin-1 regulates the PAR1-dependent signaling specificity of coagulation proteases. We have also discovered that proinflammatory reactions are dramatically up-regulated by polyphosphates, secreted by activated platelets, through interaction with nuclear proteins and inducing signaling through pathogen-associated pattern recognition receptors; toll-like receptors (TLR) 2 and 4 and the receptor for advanced glycation end products (RAGE), thereby activating mTOR/Wnt/β-catenin signaling pathways in vascular endothelial cells. We have demonstrated that coagulation proteases modulate these signaling pathways through activation of PAR1. These questions are currently being investigated by our laboratory.
In another project, we investigate mechanisms through which antithrombin regulates both anticoagulant and antiinflammatory pathways. Antithrombin (AT), as a major member of the serine protease inhibitor (serpin) family of protease inhibitors, neutralizes the enzymatic activity of all clotting proteases by directly binding their active-sites, thereby trapping them in the form of inactive complexes. The inhibitory activity of AT is greatly enhanced when it binds to the heparin-like molecules that are attached to selected vascular cell surface receptor proteins that are collectively referred to as heparan sulfate proteoglycans (HSPGs). This is the basis for the widespread use of heparin, as the primary anticoagulant drug in the treatment of thrombotic complications. We have made significant contributions to the mechanism by which AT and heparin function as anticoagulants. Recent results have indicated that the interaction of an exposed basic helix (D-helix) of AT with specific vascular HSPGs initiates antiinflammatory signaling responses that are required for the regulation of vascular integrity in health and disease. It has been hypothesized that the interaction of AT with HSPGs is also required for the conformational activation of AT, facilitating its interaction with the active-site pocket of coagulation proteases. Mutations in D-helix interfering with the AT interaction with vascular HSPGs are associated with increased risk of thrombosis. Thus, AT, similar to APC, interfaces the coagulation cascade with inflammatory pathways. The D-helix-dependent antiinflammatory signaling mechanism of AT is poorly understood. We and others have demonstrated that the interaction of AT with vascular HSPGs leads to prostacyclin (PGI2) production and down-regulation of expression of genes regulated by the NF-κB signaling pathway. We also demonstrated that interaction with the 3-O-Sufate containing HSPG named Syndecan 4 is required for the antiinflammatory signaling function of AT. Interestingly, Syndecan 4 also functions as a co-receptor for the basic fibroblast growth factor (FGF2) receptor. The mechanism by which the occupancy of Syndecan 4 by two different ligands (AT and FGF2) elicits distinct intracellular signaling responses in vascular endothelial cells is not understood and this is an active area of investigation in our laboratory.
Our laboratory is employing cellular and animal models to understand mechanisms through which the components of the two protein C and antithrombin anticoagulant pathways described above regulate coagulation and inflammation. A deficiency in the component of either pathway can be associated with pathogenesis of cardiovascular and inflammatory diseases including atherosclerosis, severe sepsis and cancer.
Brief CV
Education
M.A., Harvard University, Cambridge, MA, 1986
Ph.D. Boston University, Boston, MA, 1989
Postdoc, Howard Hughes Medical Institute, Oklahoma City, OK, 1994
Other Activities
Member of Hemostasis and Thrombosis study section, 2007-2011
Ad hoc member of numerous NHLBI Special Emphasis Panel, RFA and PPG study sections
Reviewer of grants for national and international funding organizations
Reviewer for major scientific journals
J Thromb Haemost Advisory Board, 2009-present
Enzyme Research Editorial Board Member, 2014-present
Science Advances Associate Editor, 2017-present
Memberships
American Society of Hematology
International Society of Thrombosis and Hemostasis
Joined OMRF scientific staff in 2017
Publications
Recent Publications
Biswas I, Kudo M, Rezaie AR. Endothelial Protein C Receptor and Thrombomodulin Facilitate Protease-Activated Receptor 1 Cleavage at Arginine-46 by Thrombin and Activated Protein C. J Biol Chem:110339, 2025 June, PMID: 40480637, PMCID: PMC12269503
Biswas I, Panicker SR, Lupu F, Rezaie AR. Physiological significance of antithrombin D-helix interaction with vascular GAGs. Blood Adv, 2024 December, PMID: 39671300, PMCID: PMC11907474
Aleman M, Arepally GM, Baglin T, Buitrago L, Davizon-Castillo P, Dayal S, Flick MJ, Gerber G, Hisada Y, Kolev K, O'Loghlen A, Rezaie AR, Sparkenbaugh EM, Stavrou EX, Ünlü B, Vercellotti GM. Coagulation and platelet biology at the intersection of health and disease: illustrated capsules of the 11th Symposium on Hemostasis at the University of North Carolina. Res Pract Thromb Haemost 8:102395, 2024 April, PMID: 38699410, PMCID: PMC11063502
Selected Publications
Giri H, Panicker SR, Cai X, Biswas I, Weiler H, Rezaie AR. Thrombomodulin is essential for maintaining quiescence in vascular endothelial cells. Proc Natl Acad Sci U S A. 2021 Mar 16;118(11):e2022248118. doi: 10.1073/pnas.2022248118. PMID: 33836597, PMCID: PMC7980409
Panicker SR, Biswas I, Giri H, Cai X, Rezaie AR. PKC (Protein Kinase C)-δ Modulates AT (Antithrombin) Signaling in Vascular Endothelial Cells. Arterioscler Thromb Vasc Biol. 2020 Jul;40(7):1748-1762. PMID: 32404004, PMCID: PMC7316612
Lu Y, Mehta-D'souza P, Biswas I, Villoutreix BO, Wang X, Ding Q, Rezaie AR. Ile73Asn mutation in protein C introduces a new N-linked glycosylation site on the first EGF-domain of protein C and causes thrombosis. Haematologica. 2020 Jun;105(6):1712-1722. PMID: 31399531, PMCID: PMC7271577
Lu Y, Giri H, Villoutreix BO, Ding Q, Wang X, Rezaie AR. Gly197Arg mutation in protein C causes recurrent thrombosis in a heterozygous carrier. J Thromb Haemost. 2020 May;18(5):1141-1153. PMID: 32078247, PMCID: PMC7192786
Cai X, Biswas I, Panicker SR, Giri H, Rezaie AR. Activated protein C inhibits lipopolysaccharide-mediated acetylation and secretion of high-mobility group box 1 in endothelial cells. J Thromb Haemost. 2019 May;17(5):803-817 PMID: 30865333, PMCID: PMC6494677
Biswas I, Panicker SR, Cai X, Mehta-D'souza P, Rezaie AR. Inorganic Polyphosphate Amplifies High Mobility Group Box 1-Mediated Von Willebrand Factor Release and Platelet String Formation on Endothelial Cells. Arterioscler Thromb Vasc Biol. 2018 Aug;38(8):1868-1877. PMID: 29930000, PMCID: PMC6202171
Contact
Cardiovascular Biology Research Program, MS 45
Oklahoma Medical Research Foundation
825 N.E. 13th Street
Oklahoma City, OK 73104
Phone: (405) 271-4711
Lab: (405) 271-4743
Fax: (405) 271-3137
Email: Ray-Rezaie@omrf.org
For media inquiries, please contact OMRF’s Office of Public Affairs at news@omrf.org.
Lab Staff
Mia Pederson-Rambo
Project Coordinator I