The National Institutes of Health has selected the Oklahoma Medical Research Foundation to lead a nationwide public-private partnership aimed at developing more effective treatments for autoimmune diseases.
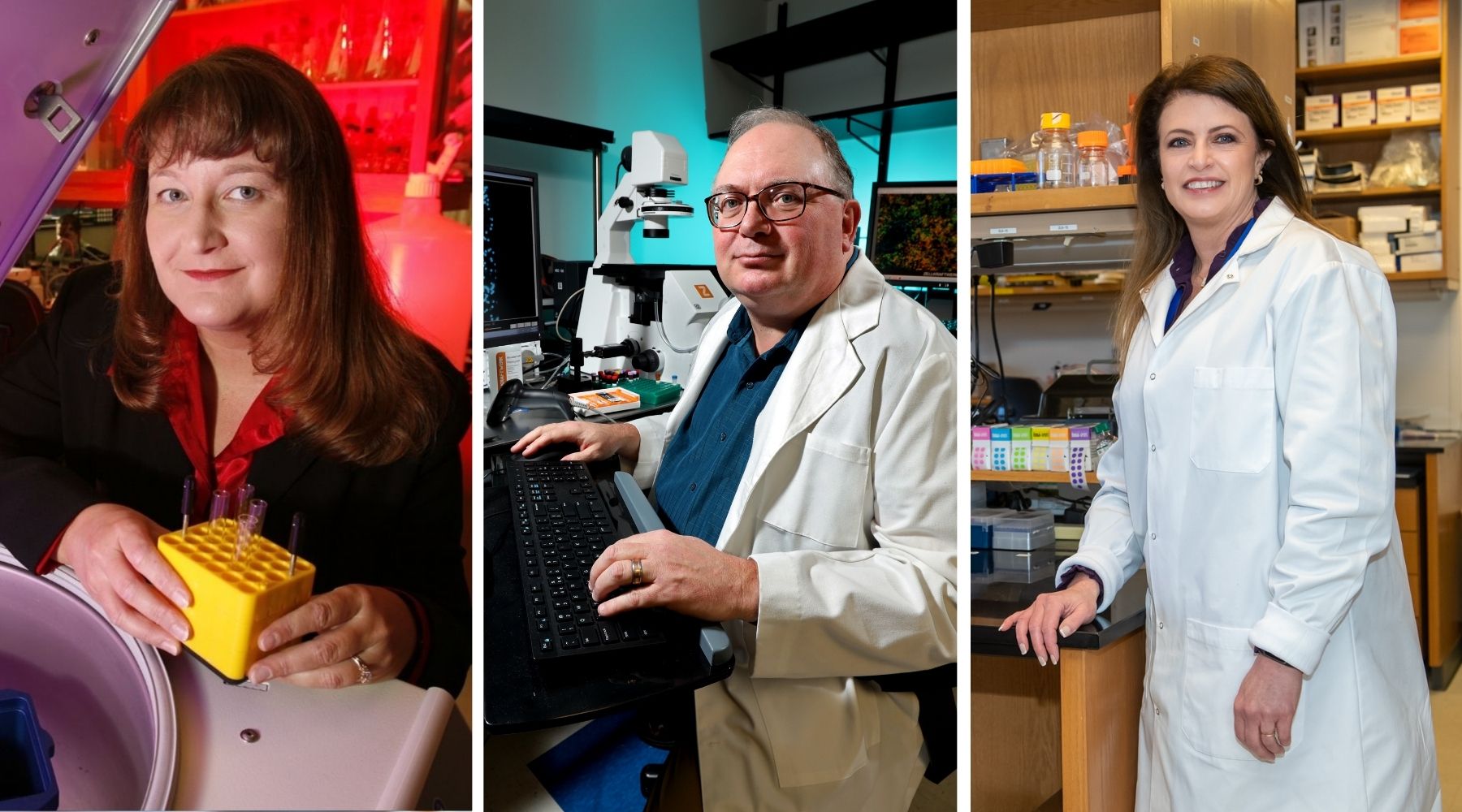
OMRF scientists Joel Guthridge, Ph.D., and Judith James, M.D., Ph.D., were awarded grants totaling more than $18.5 million to provide the leadership, expertise and infrastructure for the NIH’s Accelerating Medicines Partnership in Autoimmune and Immune-Mediated Diseases (AMP AIM). James, OMRF’s vice president of clinical affairs, is also chair of the $58.5 million program.
OMRF will manage the clinical research operations, tissue research center, centralized testing and initial spatial tissue characterization for the five-year project. Additionally, the foundation will administer a program to develop emerging technologies to better understand and treat autoimmune conditions, including lupus, rheumatoid arthritis, psoriatic-spectrum diseases and Sjögren’s disease.
Researchers in OMRF’s Arthritis and Clinical Immunology and Genes and Human Disease Research Programs are also members of one of AMP’s four disease teams. Darise Farris, Ph.D., is a co-lead investigator of the Sjögren’s Disease Team, which includes OMRF’s Chris Lessard, Ph.D., Astrid Rasmussen, M.D., Ph.D., and Hal Scofield, M.D., and scientists from the University of California, San Francisco, Johns Hopkins University and the NIH.
“Developing a new drug to treat a disease typically takes a decade or longer, and less than 5% make it to FDA approval,” said James, who holds the Lou C. Kerr Endowed Chair in Biomedical Research at OMRF. “Ultimately, this partnership seeks to identify new therapy targets for one or multiple autoimmune diseases by understanding the diseases at the individual cell level within the targeted organs.”
The AMP AIM partnership involves the NIH, Foundation for the National Institutes of Health, nonprofit disease foundations, biopharmaceutical and life-science companies, and 52 research institutions.
OMRF’s biorepository was the central repository for a previous AMP limited to lupus and rheumatoid arthritis. That partnership focused on deconstructing lupus and rheumatoid arthritis by concentrating on single-cell analyses of gene and protein expression. The new partnership will reconstruct disease at the tissue level through advanced imaging and translational analytics of clinical characteristics and molecular biomarkers to deepen the patient’s overall precision medicine profile.
“Studying a suite of disorders will enable AMP AIM investigators to conduct cross-disease comparisons that may help us pinpoint those cells and pathways that are specific to each of these diseases and those that are shared,” said Robert H. Carter, M.D., deputy director of the National Institute of Arthritis and Musculoskeletal and Skin Diseases, a part of the NIH.
Guthridge, the lead investigator on OMRF’s tissue research award, said AMP AIM offers exciting challenges and opportunities to work at the bleeding edge of research in these areas.
“This program promises to provide the most detailed information to date about immune cells that are in the tissue, exactly where those cells are located, other nearby cells, and how all those cells interact to cause inflammation and disease,” said Guthridge.
In James’ role as AMP AIM chair, she will bring together exceptional scientists, cutting-edge technologies and commercial partners into a collaborative team.
“Our role in this project is a recognition of our reputation at OMRF as a leader in autoimmune disease research,” said James. “This partnership will demonstrate that a team approach to science enables the network to achieve more than any single member or institution.”
Launched in 2014 by the NIH, AMP is intended to transform the current model for developing new diagnostics and treatments. Other target areas of the AMP program include Alzheimer’s, Parkinson’s, schizophrenia and Type 2 diabetes. Partners share a common goal of increasing the number of diagnostics and medications for patients and reducing the time and cost of developing them.
Other OMRF scientists involved in the work include Joan Merrill, M.D., Caleb Marlin, Ph.D., Miles Smith, Ph.D., Carla Guthridge, Ph.D., Kyle Wright, M.D., Ph.D., Susan Macwana, Nancy Redinger and Wade DeJager.
The grants, 1UC2AR081032-01 and 1UC2DE032254-01, are funded by the FNIH, the National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institute of Allergy and Infectious Disease, National Institute of Dental and Craniofacial Research, and the Office of Women’s Health, each of which is part of the NIH.