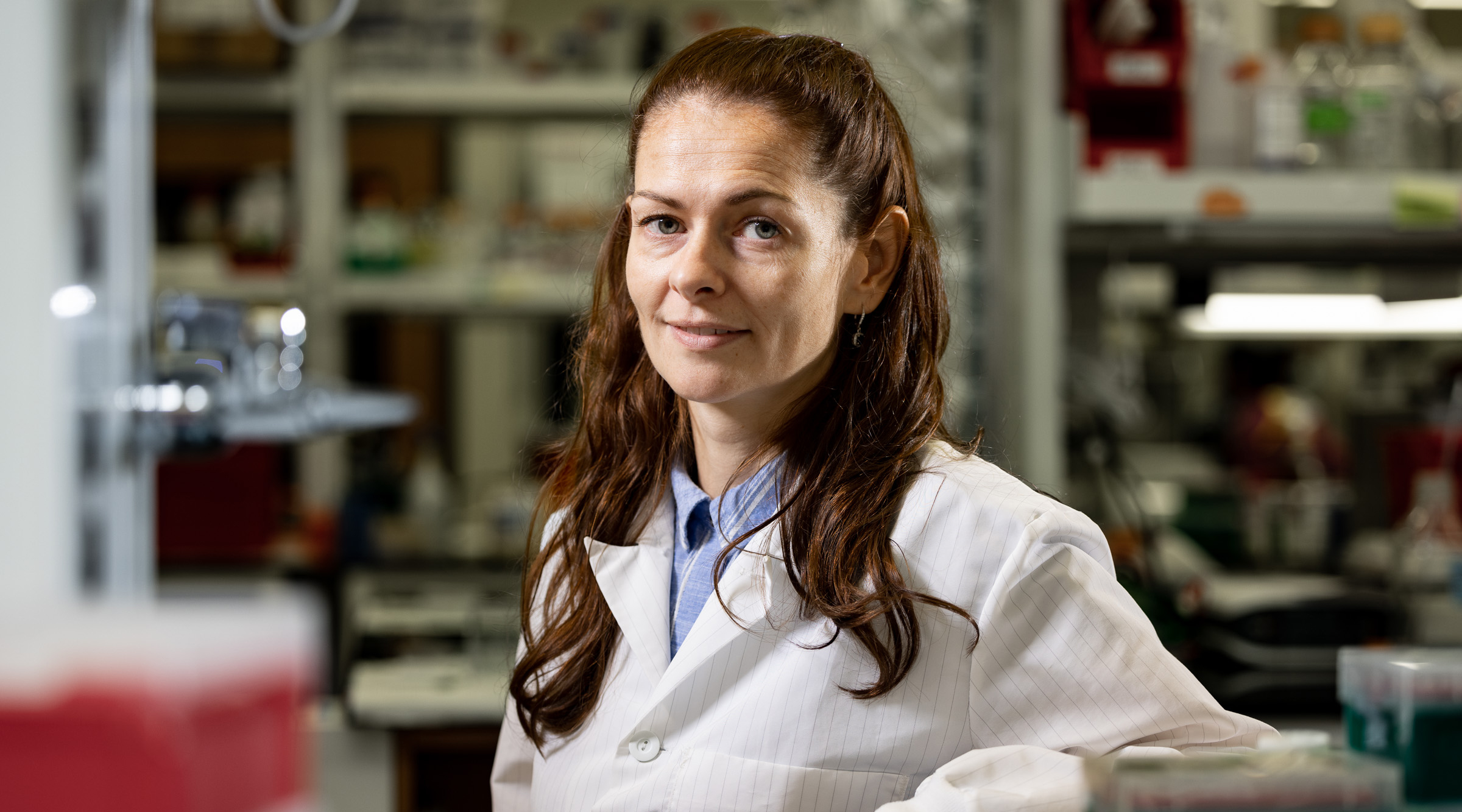
Magdalena Bieniasz, Ph.D.
Assistant Professor
Aging & Metabolism Research Program
My 101
Statistics show that epithelial ovarian cancer remains the most deadly of all gynecologic tumors, and only 46% of patients will survive for at least 5 years after diagnosis. There is a number of reasons why ovarian cancer has such a poor prognosis. One reason is that due to lack of specific symptoms, the majority of women are diagnosed at advanced stages of ovarian cancer, where cancer cells have spread from the ovary to other tissues in the abdomen. Another is that the cancer cells which survived the surgery have become resistant to chemotherapy and cancer grows back. Treatment of advanced ovarian cancer is difficult. Although surgeons do their best to make sure that all the cancer cells are removed during surgery, it is always possible that a tiny group of cancer cells has been left behind. Giving chemotherapy following surgery helps to catch any remaining cancer cells and kill them. However, it is unlikely that cancer treatment will kill every single cancer cell in the body. In addition, as a result of mutation of certain genes in cancer cells, these cells become resistant to chemotherapy. If this happens ovarian cancer patients may receive a different type of treatment. Unfortunately, very often cancer cells develop a resistance to many drugs at the same time, which makes eradication of cancer very difficult or even not possible.
My overall research program is designed to understand the function of molecules that drive ovarian cancer growth and spreading to different tissues. We also study the genetic changes in cancer cells leading to chemotherapy resistance. In addition, to ensure that we have the correct tools to study ovarian cancer as it exists in real patients, in the Bieniasz Lab we generate the most innovative and clinically relevant ovarian tumor models called patient-derived xenografts (PDXs). These tumor models are derived directly from ovarian cancer patients undergoing therapy in the Stephenson Cancer Center in Oklahoma City. PDX tumor models faithfully represent the original patient tumor features such as histology, gene expression profile (activation and mutation of specific genes) and response/resistance to therapy. We use PDX tumor models to improve preclinical evaluation of new anti-cancer therapies towards more personalized medicine. Ultimately, we aim to advance the knowledge of the mechanisms of ovarian cancer progression and chemotherapy resistance to design new treatment strategies with the long-term goal of translation of these therapies into clinical practice.