February
Two days before he almost died, Ryan Eisner felt great. In fact, if you’d asked him, Eisner, then about to begin his junior year as a point guard for the Drew University basketball team in New Jersey, would’ve told you he was in the best shape of his life.
But when a seemingly routine respiratory infection became septic, Eisner’s doctors had to intubate him and place him in a medically induced coma. “You’d better start praying,” one of the physicians told his father. “He’s going to die.”
Fortunately, Eisner didn’t. Yet the drug that saved him – Xigris, based on the work of OMRF’s Drs. Chuck Esmon and Fletcher Taylor – was eventually pulled from the market. In the time since, no other treatments have emerged. That has left patients with few therapeutic options. As a result, sepsis is the leading killer in intensive care units in the U.S., claiming an estimated 270,000 lives each year.
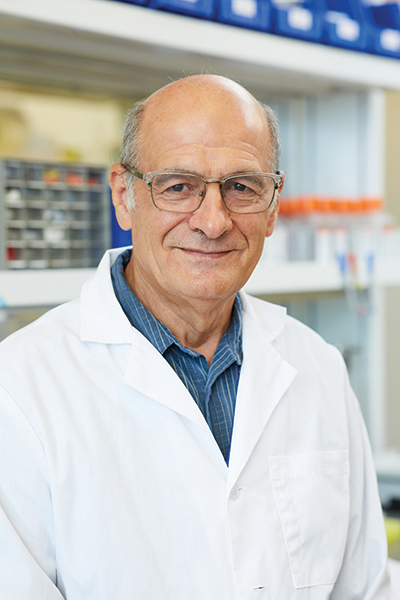
In February, OMRF’s Dr. Florea Lupu received a five-year grant to study the condition, which occurs when the immune system overcompensates while fighting a pathogen like a virus or bacteria. “We are targeting a specific part of the immune system called the complement system, which helps clear away bacteria in early sepsis but then becomes detrimental and contributes to organ failure,” says Lupu.
In particular, he’s aiming at a protein known as C5, using an investigational drug to counter the protein. “The timing for an inhibitor is crucial,” he says. “If you try to block C5 too early, you also block the clearance of bacteria. If you go in too late, the damage will already be done.”
Once sepsis becomes severe, a state technically known as shock, the odds of survival decrease by 8% for each hour of delay in treatment, says Lupu. “So, that’s the biggest challenge: finding the narrow window to a successful outcome.”
The hope is that Lupu’s research will one day bring more stories like Eisner’s. Until then, Eisner, now healthy, knows he was fortunate. “There’s not a day that I don’t think about it,” he says.