Clinical Immunology Laboratory
About
The OMRF Clinical Immunology Laboratory, under the direction of Dr. Judith James and Myositis Director Dr. Ira Targoff, performs a variety of tests to identify autoantibodies for the diagnosis and treatment of autoimmune and other diseases. On average, the Laboratory processes more than 300 samples per week. This national reference lab is CLIA-approved (Clinical Laboratory Improvement Amendments) and CAP-certified (College of American Pathologists). The most highly utilized test in the Laboratory is the Reichlin Profile, which was developed by OMRF pioneering scientist Dr. Morris Reichlin. Also known as the Lupus Profile, it is the definitive test for autoimmune disease and consists of the following sub-tests:
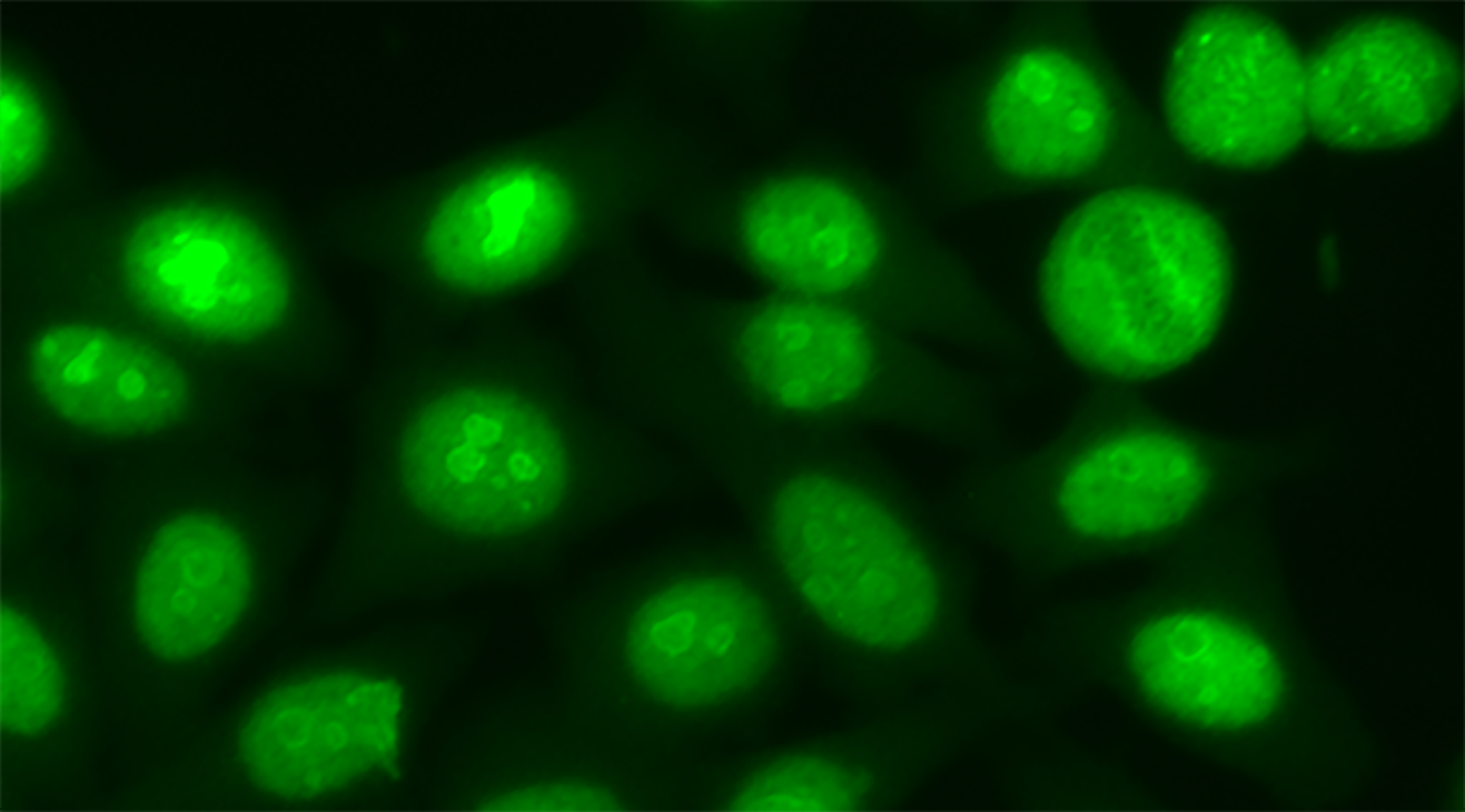
- ANA – Antinuclear antibodies are present in many rheumatic diseases and often are not specific to one single disease. They are present in over 95% of SLE patients, 86% of scleroderma patients, and in lower frequencies in rheumatoid arthritis (RA), Sjögren’s syndrome, and polymyositis.
- dsDNA – Anti-double strand DNA at a titer of 1:10 or more strongly suggests SLE.
- ENA – Extractable nuclear antibodies (precipitating antibodies) have definitive diagnostic information. Precipitating antibodies to soluble tissue antigens are present in diverse rheumatic diseases:
- anti-Sm is highly specific for SLE
- anti-nRNP (nuclear ribonucleo- protein) is present in SLE and overlap syndromes with scleroderma and polymyositis
- anti-Scl-70 is highly specific for scleroderma
- anti-Ro and anti-La are associated with SLE and Sjögren’s syndrome
- anti-P (Ribosomal P) is a new specificity related to psychosis in SLE patients and may be enriched in patients with nephritis and unexplained hepatitis
- anti-Jo-1, anti-PM-Scl and anti-Mi-2 may be seen in polymyositis patients.
Precipitating antibodies are detected by the formation of precipitin lines in agar gel against calf thymus extract (CTE) or rabbit thymus extract (RTE) for anti-Scl70. When a line does not show identity with known antibodies against tissue extracts, the precipitin is called UIL (unidentified line). By this, an association with “rheumatic disease” is recognized, but the specificities are unknown. When polymyositis is suspected, a more sensitive and definitive method known as immunoprecipitation is indicated for the detection of myositis-specific antibodies that may be present at levels too low to be detected by ENA.
Additional Testing performed by the Clinical Immunology Laboratory
- ANCA (anti-neutrophil cytoplasm antibody) detects autoantibodies against neutrophil-specific antigens. cANCA (cytoplasmic), is highly specific for necrotizing vasculitis and is present in more than 90% of biopsy-proven Wegener’s granulomatosis but also in classical polyarteritis nodosa and Churg-Strauss’ syndrome. pANCA (perinuclear) is less specific than C-ANCA but is present in a high proportion of cases of crescentic glomerulonephritis and microscopic polyarteritis nodosa. There are numerous antigens associated with both cANCA and pANCA. PR3 (serine protease3) and MPO (myeloperoxidase) are available to help further define autoimmune vasculitis disorders.
- Anti-DFS70 (dense fine speckled) responses, when found without other autoimmune rheumatic disease-specific autoantibodies, are most common in healthy individuals. Isolated anti-DFS70 antibodies are detectable in less than 1 % of autoantibody associated rheumatic diseases (AARD) but are detectable in 2-22 % of healthy persons. In the presence of an isolated anti-DFS70 antibody, the posttest probability for AARD is reduced significantly; however, the presence of the autoantibody must be put in the context of the individual clinical picture.**
- aPL (antibodies to phospholipid) are associated with recurrent fetal loss and recurrent thromboses and strokes. aPL can be found in SLE as well as non-SLE patients. Conditions with positivity include migraines, peripheral vascular disease, and some autoimmune cases of myocardial infarction and post-bypass graft thromboses.
- CCP (cyclic citrullinated peptides), a new test for the early detection of rheumatoid arthritis. Antibodies predict erosive disease and are present in 30-40% of seronegative RA.
- Cryoglobulins may indicate or be used to monitor autoimmune disease activity. These results must be interpreted in the context of the individual clinical case.
- Myositis profile – Tests for 12 antibodies specific to or associated with polymyositis and dermatomyositis
* Lab-developed test (LDT) development and performance characteristics were determined by the OMRF Clinical Immunology Laboratory to perform clinical high-complexity testing. Lab-developed tests have not been cleared or approved by the FDA. Lab-developed tests are accredited by the College of American Pathologists (CAP). References available upon request.
**This test was developed and its performance characteristics determined by the OMRF Clinical Immunology Laboratory. It has not been cleared or approved by the U.S. Food and Drug Administration. The FDA has determined that such clearance or approval is not necessary.
Research/Clinical Accounts and Billing/Insurance Inquiries
For more information, please call Misty Mihelich at 405-271-3173.
Fax number (405) 271-7524.
To contact the OMRF Clinical Laboratory staff, please call (405) 271-7771.