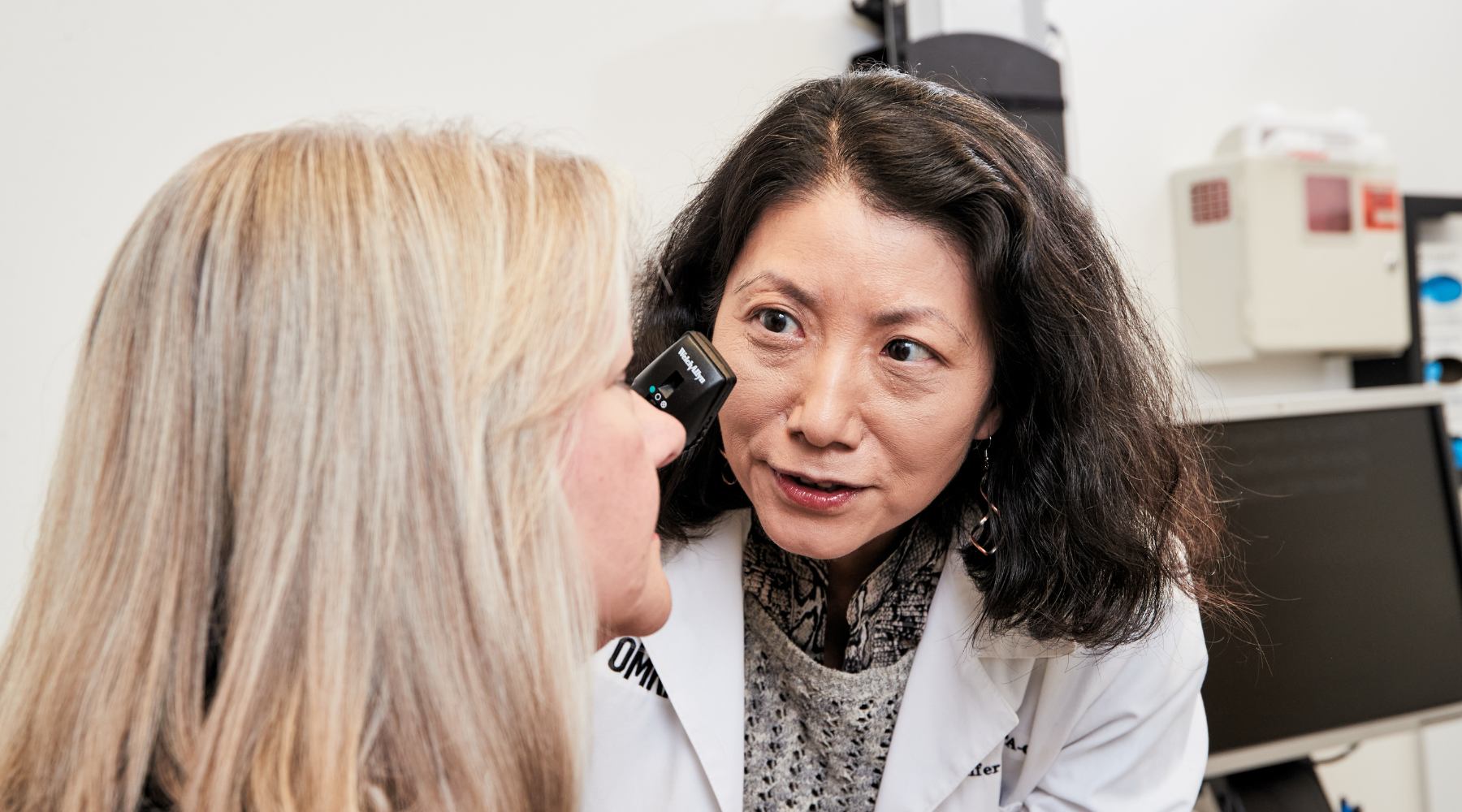
Yang Mao-Draayer, M.D., Ph.D.
Director of Clinical and Experimental Therapeutics, OMRF Multiple Sclerosis Center of Excellence
Professor
Arthritis & Clinical Immunology Research Program
Professor of Microbiology and Immunology, Professor of Pathology, University of Oklahoma College of Medicine
My 101
During my neurology residency training, I treated people with stroke, epilepsy, neuromuscular disorders, Parkinson’s, Alzheimer’s and multiple sclerosis. I was particularly intrigued by our ability to help people with MS recover fully after an active disease relapse. I was also drawn to the science of MS and neuroimmunology. MS relapse recovery is a prime example of brain plasticity – the brain’s ability to bounce back after injury. When I started my career 20 years ago, there were only three injectable medications for treating MS; now, we have nearly twenty treatment options. Despite great relapse management, some patients still become worse with more difficulty balancing, walking and thinking clearly over time. Currently there is no cure for MS. While treating patients is about meeting their immediate needs, research addresses unmet needs and improving treatment in years to come. That’s why I direct my research to understanding the potential causes and discovering cures for MS and related disorders.
My lab’s work focuses on understanding how current and future treatments affect the immune system and finding ways to repair damaged neurons. We also aim to develop precision medicine, observing an individual’s biomarkers to predict disease activity and ideal treatment.
MS onset usually comes at the prime time of life. I have been particularly touched by patients my age; from all of them, I learned resilience and perseverance. The greatest joy for me is to getting patients on the right treatment and making them feel better so that they can achieve more in their lives. Nothing is more rewarding than seeing patients do well and live happy and productive lives, a passion that the entire MS Center team shares. We not only provide thorough care to our patients but also conduct cutting-edge research to advance the treatment of MS and other related disorders. Being a physician-scientist is challenging but rewarding as we strive to make a difference in patients’ daily lives and for future scientific breakthroughs.
Research
As a professor and director of clinical and experimental therapeutics, I lead a translational molecular and cellular neuroimmunology research program. We aim to understand neuroimmunologic mechanisms and apply novel therapeutics in central nervous system demyelinating diseases, including multiple sclerosis, neuromyelitis optica and myelin oligodendrocyte glycoprotein antibody disease, known as MOGAD.
My lab pursues bench-to-bedside-and-back translational and clinical studies. We have established MS and other neuroinflammatory disease biorepositories and conducted comprehensive immunological studies on immune cells in MS. Our studies span from the analysis of immune cell type and function to biomarker discovery for disease flares and progression, as well as early disease-initiating mechanisms and the mechanisms of current MS drugs.
Disease Initiation: How do genetic and environmental factors, including smoking, infection and the microbiome, impact disease onset?
Disease Treatment: What are the mechanisms of current disease-modifying therapies, predictors of relapse, and treatment responses?
- My lab has initiated, designed and participated in groundbreaking clinical trials. We have recruited MS patients for clinical trials and mechanistic studies for lab-based deep immunophenotyping and functional studies for biomarker and therapeutic discoveries. To accomplish our goals, we use state-of-the-art technologies: OLINK, single cell analysis (RNA seq and ATAC seq) of immune cells in the peripheral blood and in the CNS (CSF and brain tissue), combined with microbiome, metabolome and MRI and OCT imaging.
- Our studies on several MS disease-modifying therapies showed they promoted a tolerogenic environment by shifting the balance between activated pathogenic and naïve or immunosuppressive immune cell subsets.
- Our recent work on costimulatory molecules led discovery of CD40L as a predictive biomarker in MS disease progression. Furthermore, we conducted investigator-initiated phase I study using humanized monoclonal antibody to CD40L in MS patients and demonstrated its safety and potential in preventing clinical and MRI disease progression.
Disease Progression: How can we slow or stop the progression of MS and related disease?
- I served as a primary project principal investigator, protocol chair and director of neuroscience research of the Autoimmunity Center of Excellence at the University of Michigan, funded by the National Institutes of Health. My lab led the central neuroimmunology lab of the ACE and collaborated with NIH, industry and 15 academic centers to ensure proper human sample collection, processing, and data analysis. Our ACE study provided immunological and molecular insights into MS disease progression.
One of the reasons I decided to join OMRF is that it combines top-notch patient care and innovative science. Through the ACE, I had the privilege of knowing other autoimmunity experts at OMRF. My goal is to broaden the scope of autoimmune disease research in collaboration with other experts in lupus, sarcoidosis and Sjögren’s disease. Our ultimate aim is to provide a comprehensive understanding of human immune function in health and through various disease courses, not only in autoimmune but also other neurodegenerative diseases.
Brief CV
Education
M.D., Capital Institute of Medicine, Beijing, China, 1990
Ph.D., Biology, University of Iowa, Iowa City, IA, 1998
Neurology residency, Chief Resident, University of Vermont College of Medicine, Burlington, VT, 2003
Neuroimmunology/MS fellowship, University of Vermont College of Medicine, Burlington, VT, 2005
Honors and Awards
Outstanding Teaching Assistant Award, University of Iowa, 1996
Mavor Academic Achievement Award, Neurology Department, University of Vermont, 2002
American Neurological Association Travel Fellowship, 2002
Physician Neuroscientist Award, College of Medicine, University of Vermont, 2005
Summer Research Merit Award (mentor), College of Medicine, University of Vermont, 2006
Foundation of the Consortium of Multiple Sclerosis Centers MS Workforce of the Future Initiative, 2008
Alpha Omega Alpha Medical Honor Society Carolyn L. Kuckein Student Research Summer Fellowship (mentor), 2009
Summer Research Merit Award (mentor), College of Medicine, University of Vermont, 2009
George Perkins Marsh Award (mentor), Biology Department, University of Vermont, 2011
Physician Scientist Award, College of Medicine, University of Michigan, 2012
Best Paper Award, International Journal of Molecular Sciences, 2016
US Best Doctors Patients’ Choice Award, 2016
University of Michigan Making a Difference Award, 2016
Americas Committee for Treatment and Research in Multiple Sclerosis Presenter Travel Award, 2017
Federation of Clinical Immunology Societies Presenter Travel Award, 2017
University of Michigan Medical School and Peking University Health Sciences Center Seventh Annual Joint Institute Symposium Travel Award, 2017
Americas Committee for Treatment and Research in Multiple Sclerosis Presenter Award, 2019
Making a Difference Award, University of Michigan, 2022
Yoga Moves Multiple Sclerosis Leadership Award, 2023
Professional Activities
American Institute of Biological Sciences Scientific Peer Advisory and Review Services- Department of Defense, Multiple Sclerosis Review Panel 2008, 2010, 2014
Natural Sciences and Engineering Research Council of Canada Grant Reviewer, 2011
Research Excellence Grant Review, Ontario Research Fund, 2014
NIH NIAID Autoimmune Center of Excellence Plenary Member, 2014-present
National Multiple Sclerosis Society Fast Forward Grant Peer Review Committee Reviewer, 2015
Elected Member of the Neuromyelitis Optica Guthy Jackson Charitable Foundation International Clinical Consortium and Biorepository, 2015-present
Florida Department of Health Research Proposals Peer Review, 2016-2017
Session Co-chair, Microbiome in MS research, 142nd American Neurological Association Annual Meeting, 2017
International Peer Review Grant Review, Ireland Health Research Board, 2017
Chair, FLUENT Study Steering Committee, 2017-2023
Peer Review Committee, National Multiple Sclerosis Society, 2018
NIH Hypersensitivity, Autoimmune, and Immune-mediated Diseases Study Section, 2018
NIH Special Emphasis Panel NIAID Cooperative Centers on Human Immunology, 2018
Chair, North American Registry for Care and Research in MS Health Economics Outcome Research Committee, 2018-present
Associate Editor, Frontier Immunology, 2019-present
Steering Committee Member, EXCHANGE Study, 2019-present
Member of Neurosarcoid Consortium, 2020-present
Chair, National Healthcare Advisory Committee National Multiple Sclerosis Society, Michigan Chapter, 2020-2021
Steering Committee Member, Frexalimab (anti-CD40L) Study, 2020-present
Co-Chair, National Healthcare Advisory Committee National Multiple Sclerosis Society, Michigan, Ohio, and Indiana Chapter, 2021-2023
FDA Neurological Rare Disease Natural History Review Panel, 2022
National Multiple Sclerosis Society Biomedical Research Committee Review Panel, 2022-present
National Multiple Sclerosis Society Special Emphasis Panel, 2023
Journal Reviews
Multiple Sclerosis, Neurology, J Neurol Neurosurg Psychiatry, Journal of Neuroimmunology, Journal of the Neurological Sciences, Annals of Clinical and Translational Neurology, European Journal of Immunology, Frontier Immunology Journal of Immunology, Neurology-Neuroimmunology Neuroinflammation, Journal of Clinical Investigation Insight
Memberships
American Academy of Neurology
Foundation of the Consortium of Multiple Sclerosis Centers
International Society for Stem Cell Research
The American Association of Immunologists
Federation of Clinical Immunology Societies
Association of Clinical Research Professionals
Joined OMRF Scientific Staff in 2023
Publications
Recent Publications
Obeidat AZ, Betz M, Farber RS, Goff E, Gudesblatt M, Hua LH, Mao-Draayer Y, Robertson D, Santoro JD, Wang T, Gomes D, Bozin I, Mendoza JP, Bian B, Lewin JB, Belviso N, Shankar SL. Comparative Effectiveness and Risk of Severe Infection in Adult Patients With MS Treated With Diroximel Fumarate Versus Anti-CD20 Monoclonal Antibodies: A Real-World Claims Analysis. Adv Ther, 2026 February, PMID: 41706313
Swamy SN, Belury MA, Cole RM, Heitman K, Pan S, Yang Z, Karabukayeva A, Mao-Draayer Y, Hanaoka BY. Elevated Plasma Monounsaturated Fatty Acids and Their Associations with Disease Activity, Adiposity, and Sex in Patients with Rheumatoid Arthritis: A Cross-Sectional Study. medRxiv, 2026 January, PMID: 41646807, PMCID: PMC12870717
Abboud H, Steingo B, Vargas D, Patel J, Willis MA, Mao-Draayer Y, Khaitov D, Avila Ornelas J, Subei A, Reed C, Baek WS, Tsai M, Kim A, Obeidat AZ, Pandey K, Levy M, Molazadeh N, Shin RK, Romero RS, Goulette P, Walch R, Coté J, Pace R, Sengul B, Osborne B, Mahadeen A, Ferayorni L, Gholizadeh S. Satralizumab treatment in adults with aquaporin-4 immunoglobulin G-seropositive neuromyelitis optica spectrum disorder in clinical practice. Mult Scler J Exp Transl Clin 11:20552173251386895, 2025 December, PMID: 41383264, PMCID: PMC12690068
Selected Publications
Wu Q, Wang Q, Yang J, Martens JW, Mills EA, Saad A, Chilukuri P, Dowling CA, Mao-Draayer Y. Elevated sCD40L in Secondary Progressive Multiple Sclerosis in Comparison to Non-progressive Benign and Relapsing Remitting Multiple Sclerosis. J Cent Nerv Syst Dis. 2021 Oct 25;13:11795735211050712. doi: 10.1177/11795735211050712. PMID: 34720605; PMCID: PMC8552403.
Fadul CE*, Mao-Draayer Y*, Ryan KA, Noelle RJ, Wishart HA, Channon JY, Kasper IR, Oliver B, Mielcarz DW, Kasper LH. Safety and Immune Effects of Blocking CD40 Ligand in Multiple Sclerosis. Neurol Neuroimmunol Neuroinflamm. 2021 Oct 15;8(6):e1096. doi: 10.1212/NXI.0000000000001096. PMID: 34654708; PMCID: PMC8527364.
Wu Q, Mills EA, Wang Q, Dowling CA, Fisher C, Kirch B, Lundy SK, Fox DA, Mao-Draayer Y; AMS04 Study Group. Siponimod enriches regulatory T and B lymphocytes in secondary progressive multiple sclerosis. JCI Insight. 2020 Feb 13;5(3):e134251. doi: 10.1172/jci.insight.134251. PMID: 31935197; PMCID: PMC7098784.
Park J, Wang Q, Wu Q, Mao-Draayer Y*, Kim CH*. Bidirectional regulatory potentials of short-chain fatty acids and their G-protein-coupled receptors in autoimmune neuroinflammation. Sci Rep. 2019 Jun 20;9(1):8837. doi: 10.1038/s41598-019-45311-y. Erratum in: Sci Rep. 2019 Nov 20;9(1):17511. PMID: 31222050; PMCID: PMC6586800.
Wu Q, Wang Q, Mao G, Dowling CA, Lundy SK, Mao-Draayer Y. Dimethyl Fumarate Selectively Reduces Memory T Cells and Shifts the Balance between Th1/Th17 and Th2 in Multiple Sclerosis Patients. J Immunol. 2017 Apr 15;198(8):3069-3080. doi: 10.4049/jimmunol.1601532. Epub 2017 Mar 3. PMID: 28258191; PMCID: PMC5464403.
Lundy SK, Wu Q, Wang Q, Dowling CA, Taitano SH, Mao G, Mao-Draayer Y. Dimethyl fumarate treatment of relapsing-remitting multiple sclerosis influences B-cell subsets. Neurol Neuroimmunol Neuroinflamm. 2016 Mar 3;3(2):e211. doi: 10.1212/NXI.0000000000000211. PMID: 27006972; PMCID: PMC4784801.
Contact
Multiple Sclerosis Center of Excellence
Arthritis & Clinical Immunology Research Program, MS 50
Oklahoma Medical Research Foundation
825 N.E. 13th Street
Oklahoma City, OK 73104
Phone: (405) 271-7291
E-mail: Yang-Mao-Draayer@omrf.org
For media inquiries, please contact OMRF’s Office of Public Affairs at news@omrf.org.
Lab Staff
Joshua "Josh" Mytych, Ph.D.
Postdoctoral Scientist
Megan Reidy
Research Technician III
Meerah Khan
Clinical Research Coordinator
Ismail Muwenda
Graduate Student
Louise Williamson
Finance and Administrative Specialist
Nyeisha Caldwell
Administrative Assistant III