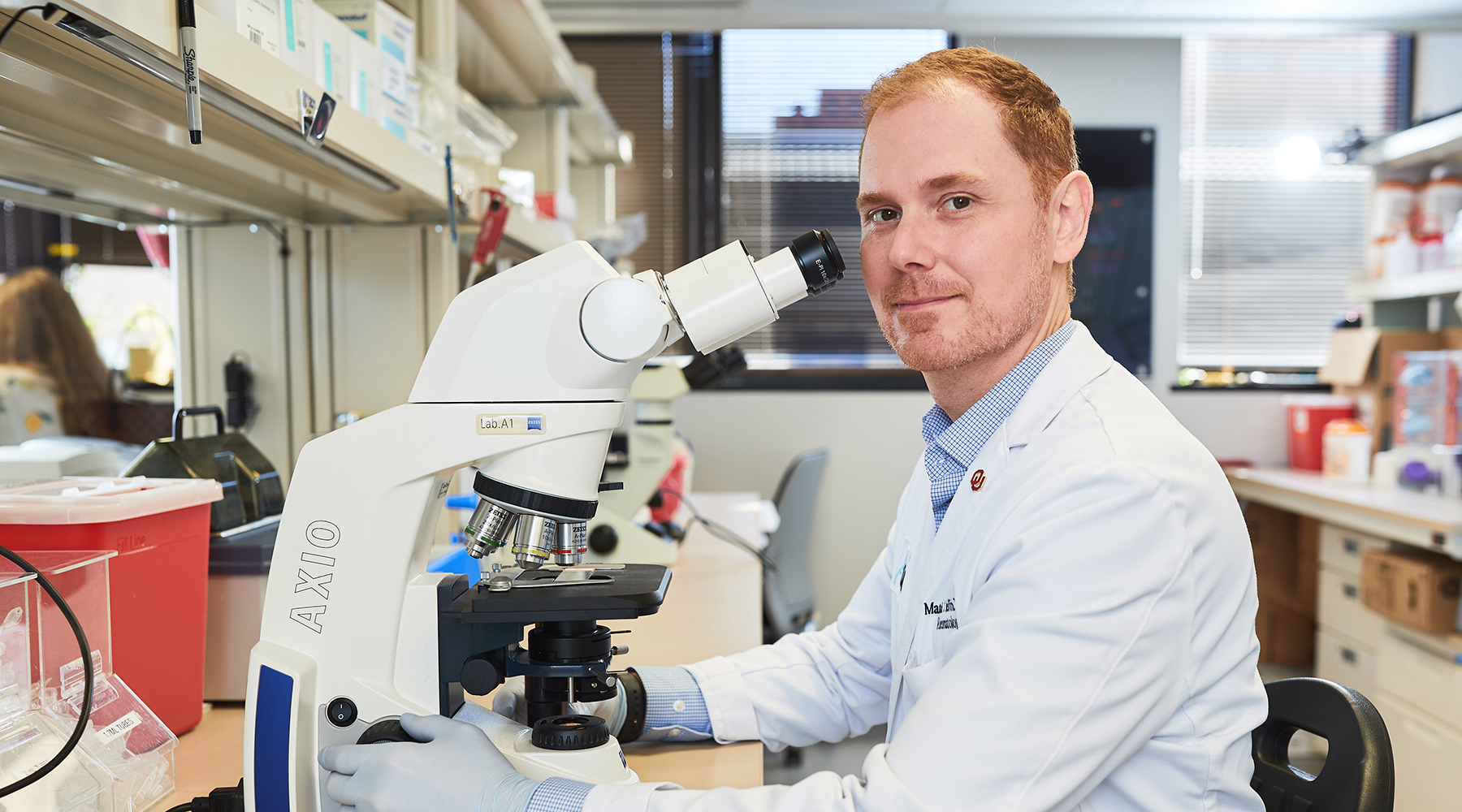
Matlock Jeffries, M.D.
OMRF Director of Arthritis Research Center
Associate Professor
Arthritis & Clinical Immunology Research Program
Clinical Associate Professor of Medicine, University of Oklahoma Health Sciences Center
My 101
Osteoarthritis (OA) is the most common form of arthritis and affects more than half of people over the age of 65 in the US. It is the most common cause of disability in our country, and the only definitive treatment for knee OA, joint replacement, is the #1 expense for Medicare each year. Despite all this, we have no medications that can slow or stop OA progression, nor do we have biomarkers to predict OA development or progression.
Unlike some other forms of arthritis, relatively few specific genetic associations have been found in OA. It seems that non-genetic, environmental factors play the biggest role in development and progression, including aging, obesity, and previous joint trauma. My laboratory is dedicated to figuring out how these non-genetic factors affect the way that cells within joints and in the immune system through epigenetic modifications. Epigenetics, meaning literally “above the gene”, are mechanisms that turn genes on and off without affecting the actual genetic code, usually by adding bits of chemical signals to DNA and other DNA-associated factors. We hope to unravel the ways in which each particular OA risk factor affects the epigenetic state of genes in multiple types of cells throughout the body in an effort to help combat this disease. We are also focusing on interventions that might “fix” these epigenetic aberrations, including through modifying the microbiome, in hopes that we might be able to prevent OA or limit its severity.
My laboratory is also interested in the microbiome in OA. We were the first to identify a microbiome within human and mouse cartilage, which changes as patients develop OA. Furthermore, we have shown that microbiome transplantation in mice can significantly improve cartilage healing, something we are following up as a potential new OA therapy.
Research
Identifying epigenetic changes associated with OA in a variety of tissues: We have previously described differential DNA methylation within OA chondrocytes and subchondral bone in specimens from end-stage OA patients. My laboratory is now focused on determining, using mouse models of OA, which genes and/or gene pathways are epigenetically modified by individual OA risk factors including trauma, advanced age, and obesity induced by high-fat diet. We hope to better define which epigenetic aberrations are potentially “reversible”, i.e. associated with diet and obesity, and which are “non-reversible”, i.e. associated with aging and prior trauma.
Using epigenetics as clinical biomarkers for OA prediction: In a pilot project based on samples from the Osteoarthritis Initiative (OAI), we demonstrated the potential to use peripheral blood mononuclear cell (PBMC) DNA methylation-based models to distinguish knee OA patients who would go on to experience rapid radiographic progression within 24 months from patients who would not progress. Building on these findings, we are now evaluating PBMC DNA methylation patterns from a large set of OAI patients based on the Foundation for the NIH (FNIH) Osteoarthritis Biomarkers Consortium to determine whether models can be developed to differentiate nonprogressors from radiographic progressors from pain progressors, and radiographic and pain progressors from each of these groups.
The microbiome and OA: A distinguishing feature of the two risk factors most strongly associated with OA, aging and obesity, is that they both are associated with changes in the gut microbiome. We are investigating the ways in which these microbiome changes affect OA progression via modulation of the immune system.
We also recently published data demonstrating that cartilage healing is partially dependent on the gut microbiome; specifically, that microbiome transplantation from 'superhealer' MRL mice to non-healer B6 mice can transfer a cartilage healing phenotype. We are now investigating the mechanisms underlying this microbiome-mediated protection.
Cartilage microbial DNA and OA: In 2019, we made a pivotal discovery in finding traces of microbial DNA within human and mouse cartilage. Moreover, we found that microbial DNA patterns from human OA patients differed from disease-free human samples, and these differences were mirrored in cartilage from OA-susceptible compared to OA-resistant mice. We are now working to determine the source of this microbial DNA signature as well as investigating its role, if any, in OA pathogenesis.
Brief CV
Education
B.S., biochemistry, University of Oklahoma, Norman, OK, 2005
M.D., University of Oklahoma Health Sciences Center, Oklahoma City, OK, 2010
Resident Physician, OUHSC Department of Internal Medicine, Oklahoma City, OK, 2010-2013
Chief Resident, OUHSC Department of Internal Medicine, Oklahoma City, OK, 2013–2014
Rheumatology Fellow, OUHSC Department of Rheumatology, Immunology, and Allergy, Oklahoma City, OK, 2014–2016
Honors and Awards
Oklahoma State Regents for Higher Education Academic Scholars Program, Oklahoma State University and University of Oklahoma, 2000-2004
Graduate Research Education and Technology Symposium Research Presentation Winner, OUHSC, 2006
Clinical and Transitional Science Award and Preceptorship, OUHSC, 2007
Special Recognition, Resident and Student Abstract Competition, American College of Rheumatology Research Workshop, 2008
Abbott Medical Student Research Preceptorship, Rheumatology Education Foundation/Association of Rheumatologic Health Professionals, 2008
Tinsley Harrison Award for best original research manuscript published in 2009, coauthor, American Journal of the Medical Sciences, 2009
Joseph E. Johnson Leadership Day Award, American College of Physicians Leadership Day, Washington, D.C., 2001
James F. Hammarsten Award, Best Oral Research Presentation, OUHSC Stewart Wolf Research Forum, 2012
Ephraim P. Engleman Endowed Resident Research Preceptorship, Rheumatology Education Foundation/Association of Rheumatologic Health Professionals, 2012
Department of Internal Medicine Medical Student Teaching Award, OUHSC, 2012
Lloyd Rader Resident Award for Excellence in Clinical Practice and Medical Research, OUHSC, 2014
Invited guest speaker, Inaugural Epigenetics of Osteoarthritis Meeting, Amsterdam, 2016
Distinguished Fellow Award, American College of Rheumatology, 2016
Junior Faculty Research Award, Plenary Speaker, Southern Society for Clinical Investigation/American Federation for Medical Research, 2018
Arthritis National Research Foundation Scholar, 2018
Invited Year-In-Review speaker, Osteoarthritis Genetics and Epigenetics, Osteoarthritis Research Society International Annual Meeting in Liverpool, 2019
Arthritis Foundation Oklahoma Chapter 2019 Professional Honoree, 2019
Session Chair, Osteoarthritis Genetics and Epigenetics, Osteoarthritis Research Society International Annual Meeting in Toronto, 2019
Provost’s Junior Faculty Research Award, OUHSC, 2019
Fred Jones Award for Scientific Achievement, OMRF, 2021
Memberships
American College of Rheumatology
American College of Physicians
Osteoarthritis Research Society International
Southern Society for Clinical Investigation
Joined OMRF scientific staff in 2020
Publications
Recent Publications
Brawner CM, Dyson G, Barrett M, Hanebutt N, Szymczak A, Mehta-D'souza P, Jeffries MA. Peripheral blood DNA methylation changes are predictive of incident radiographic osteoarthritis development: Data and biospecimens from the osteoarthritis initiative. Osteoarthr Cartil Open 7:100692, 2025 September, PMID: 41127556, PMCID: PMC12538419
Bernardini A, Taylor B, Jeffries M. Effects of Long-Term Carprofen and Omeprazole Administration in C57BL/6J Mice. J Am Assoc Lab Anim Sci:1-7, 2025 September, PMID: 40987460, PMCID: PMC12694136
Dominguez D, Vaclaw S, McClard CK, Jeffries MA, Noori J. Successful Use of Upadacitinib, a Selective JAK Inhibitor, in the Treatment of Two Cases of Recalcitrant Chronic Uveitis. J Ophthalmic Vis Res 20, 2025 May, PMID: 40689111, PMCID: PMC12258069
Selected Publications
Velasco C, Dunn C, Studrdy C, Izda V, Martin J, Rivas A, McNaughton J, Jeffries MA. Ear wound healing in MRL/MpJ mice is associated with gut microbiome composition and is transferable to non-hearler mice via microbiome transplantation. PLoS One. 2021 Jul 20;16(7):e0248322. doi: 10.1371/journal.prone.0248322. eCollection 2021. PMID: 34283837
Dunn CM, Velasco C, Rivas A, Andrews M, Garman C, Jacob PB, Jeffries, MA. Identification of cartilage microbial DNA signatures and associations with knee and hip osteoarthritis. Arthritis Rheumatol. 2020 Jul;72(7):1111-1122. Epub 2020 May 12. PMID: 31961065, PMCID: PMC7336391 (available on 2021-07-01)
Dunn CM, Nevitt MC, Lynch JA, Jeffries MA. A pilot study of peripheral blood DNA methylation models as predictors of knee osteoarthritis radiographic progression: data from the Osteoarthritis Initiative (OAI). Sci Rep. 2019 Nov 14;9(1):16880. PMID: 31727952, PMCID: PMC6856188
Jeffries MA, Donica M, Baker L, Stevenson M, Annan AC, Humphrey MB, James JA, Sawalha AH. Genome-wide DNA methylation study identifies significant epigenomic changes in osteoarthritic subchondral bone and similarity to overlying cartilage. Arthritis Rheumatol. 2016 Jun;68(6):1403-14, PMID: 26713865 PMCID: PMC5484167
Jeffries MA, Donica M, Baker LW, Stevenson ME, Annan AC, Humphrey MB, James JA, Sawalha AH. Genome-wide DNA methylation study identifies significant epigenomic changes in osteoarthritic cartilage. Arthritis Rheumatol. 2014 Oct;66(10):2804-15. PMID: 24980887
Contact
Arthritis & Clinical Immunology Research Program, MS 53
Oklahoma Medical Research Foundation
825 N.E. 13th Street
Oklahoma City, OK 73104
Phone: (405) 271-7805
Fax: (405) 271-8797
E-mail: Matlock-Jeffries@omrf.org
For media inquiries, please contact OMRF’s Office of Public Affairs at news@omrf.org.
Lab Staff
Padmaja Mehta D'souza, Ph.D.
Staff Scientist
Aleksander Szymczak, Ph.D.
Postdoctoral Scientist
Montana Barrett
Research Technician III
Cindy Brawner
Research Technician III
Pratibha Dube
Research Technician II
Gabriella "Gabby" Dyson
Research Technician II
Nicholas Hanebutt
Research Technician II
Elias Cherian
Laboratory Technician
Austin Lopez
Laboratory Technician
Nyeisha Caldwell
Administrative Assistant III