By Adam Cohen
In diseases ranging from Alzheimer’s to influenza, OMRF scientists are trying to understand the role that sex plays.
As a postdoctoral researcher at the Mayo Clinic in Minnesota, Dr. Michael Stout had his share of disagreements with his mentor.

The senior scientist, an esteemed researcher in the field of aging, had recently turned the focus of his laboratory to the deterioration cells undergo as they grow older. Stout’s job was to find ways to trigger this decline. However, despite his best efforts, he was failing. Or at least that’s what he thought.
Whenever Stout showed the results of his work, his mentor took issue. The young scientist had repeatedly proven unable to achieve the desired outcome, and his mentor contended that the fault lay not in the compound Stout had been using – a form of the female sex hormone estrogen – but, rather, in the design of his trainee’s experiments.
So, Stout set out to settle the matter once and for all.
He incorporated the compound, known technically as 17 alpha-estradiol, into a special diet. Then he fed it to 18-month-old mice and studied what happened.
Again, he found no evidence of cellular deterioration. But this time, he also saw a series of biological results that suggested almost the opposite effect.
With the estrogen supplement, the mice showed improved insulin sensitivity, a key predictor of diabetes and other metabolic illnesses. “They also had reduced fatty liver disease, reduced DNA damage and reduced body fat,” Stout says. By many measures, the animals had undergone a surprising “metabolic transformation.”
 The animals’ body clocks seemed to have rewound, and their systems for processing food and generating energy no longer resembled those of rodents in late middle age. “They looked like 6-month-old mice,” says Stout.
The animals’ body clocks seemed to have rewound, and their systems for processing food and generating energy no longer resembled those of rodents in late middle age. “They looked like 6-month-old mice,” says Stout.
Just as interestingly, the mice – all males – showed no sign the female sex hormone was causing the growth of breast tissue, reduced sperm production, loss of libido, redistribution of body fat, or loss of muscle mass. “So,” says Stout, “it appeared you could take an estrogen and get all of these metabolic benefits without feminizing effects.”
When Stout reran the experiment with female mice, though, he got very different results. Only in extremely obese animals did he see any metabolic improvement, and those changes were mild.
At first blush, the disparity appears puzzling. After all, you might presume that giving a female sex hormone to older females, whose bodies produce less of it as they age, would be beneficial. You might also ask why giving that same sex hormone to males would reverse numerous biological processes linked to advancing age.
Yet these results mirrored other experiments with the compound. When researchers fed mice a diet supplemented by 17 alpha-estradiol, males lived 20% longer. Meanwhile, it had no impact on females’ lifespans.
For Stout, who joined OMRF in 2021 as an associate professor, the work has formed a foundation for his studies going forward. “Our lab’s overarching goal is to figure out if there’s a role for sex hormones, and the receptors in the body that interact with them, in affecting disease burden in a sex-specific way.”
The idea that diseases could strike men and women differently might seem obvious. But until recently, that concept was anything but.

A Population Ignored
The 20th century marked a watershed for medical research, with a depth and breadth of discoveries and breakthroughs – antibiotics, vaccines, therapies for illnesses ranging from can
cer to cardiovascular disease – that dwarfed all that had come before. Yet the medical knowledge gathered during this time came almost exclusively from men.
For example, the National Institutes of Health launched its pioneering Baltimore Longitudinal Study of Aging in 1958 with the ambitious goal of exploring how the passage of time affects all systems in the body. However, it took another 20 years (and 1,000 research subjects) before the project enrolled its first woman.
In the 1980s, researchers at Harvard Medical School and Brigham and Women’s Hospital created the Physicians’ Health Study to examine the risks and benefits of regularly taking aspirin and various vitamin supplements. When the landmark project wrapped up, concluding that low-dose aspirin decreased the chances of a first heart attack, scientists had followed more than 22,000 research volunteers. None of them were women.
At times, the tilt toward men took research down absurd paths. After doctors observed that women tend to have lower rates of heart disease before menopause, researchers conducted the first trial of whether hormone supplementation might have a protective effect for coronary disease. The study enrolled 8,641 men and no women. Another NIH-supported project looked at how obesity affected breast and uterine cancer; again, head-scratchingly, it included only men.
As more women entered the field of research, they began to call attention to the disparity, and the NIH stepped up efforts to balance the scales. But when progress proved halting, lawmakers stepped in. “Somehow,” one representative noted during congressional hearings, “I find it hard to believe that the male-dominated medical community would tolerate a study of prostate cancer that used only women as research subjects.” In 1993, Congress mandated that all federally funded clinical research studies include women.
Still, the sex gap persisted in laboratory research, where scientists perform pre-clinical experiments involving cells and laboratory animals. Accounting for sex in these types of studies can be biologically difficult, requiring a level of specialized analysis many laboratories lack. And generating statistically reliable results for each sex drives up the time, effort and expense of experimentation, as the studies must involve a larger number of samples or subjects.
In 2016, the NIH also sought to level this playing field, enacting a policy calling for the inclusion of both sexes in studies involving cells and animals. As the largest funder of nonprofit and academic research in the world, that call appeared to make an immediate impact: A report analyzing
34 biology journals found that within a few years of the policy’s adoption, the number of pre-clinical studies that included both males and females had almost doubled.
But while the numbers looked promising on their face, a deeper analysis revealed a more nuanced picture. Specifically, while many studies reported sex differences, most failed to dig deeper in an effort to root out a biological explanation.
In neuroscience, for example, studies showed a spike in the inclusion of both males and females. However, fewer than half even broke down the results by sex. “If we’re not doing sex-based analysis,” the report’s co-author told the journal Nature, “we’re essentially leaving half the data on the table.”
Women, Men and Alzheimer’s
Dr. Sarah Ocañas became interested in neuroscience as “a little kid,” thanks to an encounter with a female neurosurgeon. “I was very inspired by her as a woman in a male-dominated field,” says Ocañas, who grew up in a small town in upstate New York.
Ocañas double-majored in mathematics and biology as an undergraduate, then joined Teach for America, a nonprofit that sends educators to underserved communities. For seven years, she taught high school calculus, statistics and anatomy in Texas’ Rio Grande Valley. “Teaching was rewarding, and I enjoyed it, but it wasn’t something I could see myself doing in the long term,” she says.
While in Texas, she also earned a master’s degree in mathematics, and one of her projects involved modeling the electrical activity of neurons. It sparked something in her. “I wanted to figure out how I could use math to solve neuroscience problems,” she says.
In 2017, she enrolled in the graduate program in neuroscience at the University of Oklahoma Health Sciences Center. It was, she says, “a very exciting time to come back to science.” Technology had improved by leaps and bounds, and data that had once taken years – and cost millions – to gather could be generated in 24 hours for a few hundred dollars. “The capabilities we had just exploded,” she says.
With the help of these new methods, her mentor, OMRF’s Dr. Bill Freeman, had detected higher levels of inflammation in the brains of healthy, older female mice than in their male counterparts. “We wanted to know what was responsible for this,” says Ocañas. For her Ph.D. dissertation, she performed a series of experiments, then used a variety of sophisticated analytical approaches to identify the culprit: microglia, a type of resident immune cell in the brain.
The work earned Ocañas a 2022 NIH Director’s Early Independence Award, the first ever given in Oklahoma and one of only 14 nationwide. Totaling $2.2 million over four years, the grant enabled her to bypass the traditional postdoctoral fellowship and open an independent research lab at OMRF, where she set out to answer a new – but related – set of questions. All of them center on one of medicine’s most intractable and devastating conditions: Alzheimer’s disease.
In America, there are nearly twice as many women as men living with Alzheimer’s. That’s partly due to the fact that there are more older women than men, and the older you are, the greater your chances of being struck by the neurodegenerative illness. But that’s not the whole story.
Studies have shown that among older women and men of the same age, women are more likely to develop Alzheimer’s. In addition, says Ocañas, women have more profound biological manifestations of the disease. “The primary hallmarks of Alzheimer’s within the brain are the accumulation of plaques and tangles, and women tend to have worse plaque buildup,” she says. “They also have worse cognitive decline.” However, she says, if men get the disease, they tend to die more quickly. “It appears that even though women experience the disease in a more aggressive way, they may also have some sort of resilience in terms of surviving.”
Ocañas is now studying the role sex chromosomes may play in the differing ways Alzheimer’s strikes women and men. From a genetic perspective, she says, it makes perfect sense that we’d see disparities.
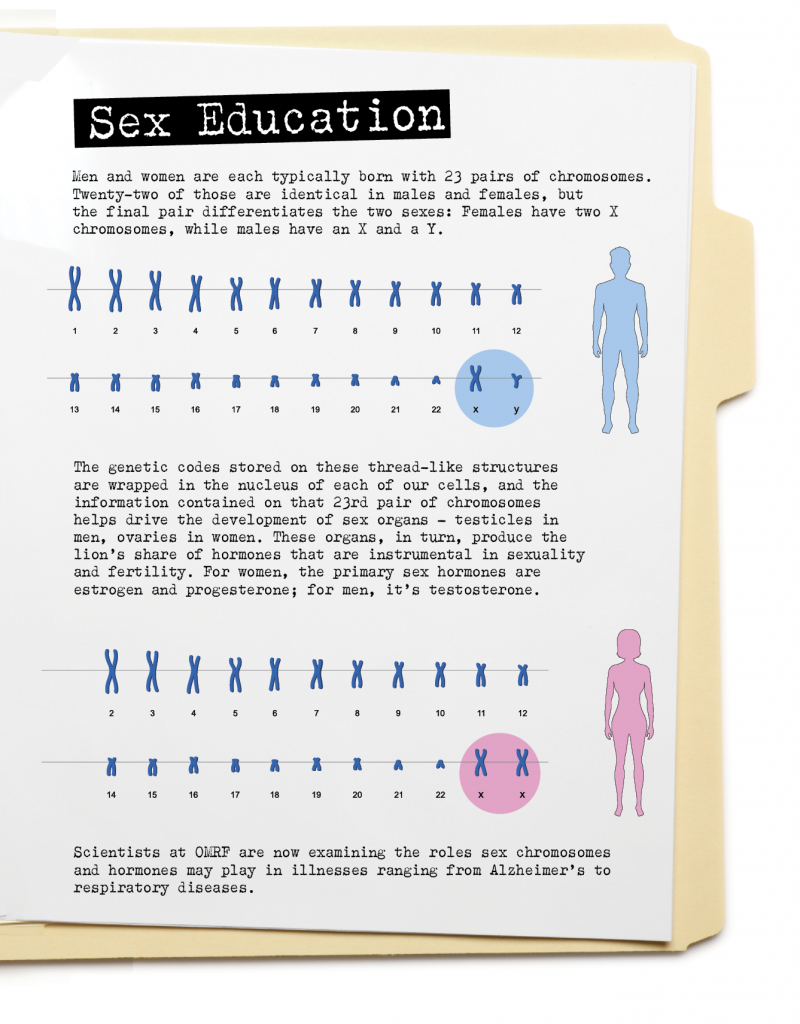
Of humans’ 46 chromosomes, males and females have 45 in common. However, each sex carries a different final chromosome, depending on whether we are female (X) or male (Y). That means the two sexes share a bit less than 98% of the genome.
Meanwhile, says Ocañas, “We are almost 99% genetically identical to chimpanzees of the same sex.” Forget about women being from Venus and men from Mars. To see the magnitude of the genetic gap between sexes, we need only visit the nearest zoo: “Men and women have more in common with chimps of the same sex than we do with one another.”
To understand sex’s part in Alzheimer’s, Ocañas is now looking more deeply at the ways in which the chromosomes vary between males and females. “We want to know how those could be contributing to the differences we see in the brain,” she says. Specifically, she’s examining how they may cause microglia, the resident immune cells, to become activated, a process that appears linked to the cognitive decline that comes with Alzheimer’s.
With a new grant from the Alzheimer’s Association, she’s also investigating how the steep decline in sex hormones as women age may impact Alzheimer’s. “Menopause,” she says, “has historically been neglected in studies.” Her lab will probe whether the loss of estrogen that accompanies menopause could be a driver behind Alzheimer’s higher incidence and disease burden in women.
In the longer term, she aims to explore whether she can identify certain groups of women for whom hormone replacement therapy might help prevent or treat Alzheimer’s. “If we’re going to find an effective intervention, it’s not going to be one-size-fits-all,” she says. “It’s going to have to be a more personalized approach where we’re taking into account sex, hormone status and genetics.”
Today, when a woman sees a doctor, that physician likely will have learned using models of disease developed primarily by studying men. One of Ocañas’ ultimate goals is to help correct that imbalance. “If clinicians are trained on the biological sex differences in disease,” she says, “then they can provide equitable healthcare to men and women.”
The Weaker Sex?
The immune system is one of those areas where men and women are not created equal. A complex network of biological systems that includes the bone marrow, skin, spleen and thymus, it protects the body from viruses and bacteria. But when the body is called to fight off outside invaders, men are the weaker sex. For many years, though, medical researchers believed the opposite.
In studies of influenza, they observed that women consistently experienced more severe symptoms than men. For that reason, scientists concluded that female immune systems must lag their male counterparts.
Then came Covid-19. As with so many aspects of science, the virus caused researchers to rethink their ideas about sex differences and immune response.

Once again, they saw that women often fared worse in the early phases of infection. But, says OMRF immunologist Dr. Susan Kovats, scientists realized that rather than highlighting a weakness, the pronounced symptoms signaled a more robust immune response.
“If you feel crappy, it’s not because you’re failing to get rid of the virus. It’s because your immune response is really strong,” says Kovats. When researchers went back and reexamined their studies of flu, they found the same thing. What’s more, they determined that the worst symptoms appeared in women in their reproductive years.
To Kovats, who studies how sex-related hormones impact immune responses, this made sense. “During reproductive years, women have a lot of estrogen,” she says. She hypothesizes that the female sex hormone may fuel women’s more vigorous immune responses. It could also help explain why female immune systems seem to respond more effectively to Covid vaccines – and why, with the loss of estrogen, the virus becomes more dangerous as women age.
However, the increasing severity of Covid and other respiratory viruses as we grow older is not limited to women. Again, says Kovats, that’s unsurprising, as men also experience a drop-off in male sex hormones like testosterone as they grow older. While that decline follows a more gradual curve than the sudden hormonal cliff women experience with menopause, the end result is the same: a loss of protection and other benefits sex hormones offer.
Because men’s immune systems start at a disadvantage, says Kovats, they also end at one when they reach their 70s, 80s and beyond. “Because of the loss of testosterone, along with the natural reduction of the ability to produce interferon” – a protein that inhibits virus replication – “elderly men do the worst” with Covid and other respiratory infections like it.
In her lab, Kovats and her research team are studying how estrogen affects immune cells and changes the way they function. “If we know how women and men respond differently, then we might be able to figure out therapeutic approaches that allow us to manipulate different immune pathways,” she says. Like her colleague Ocañas, she sees sex differences as a key to unlocking the effectiveness of treatments, both existing and new. “If men and women have different immune pathways when they are sick or they get
an infection, can we find different treatments that target those pathways?”
Similarly, decades spent parsing the relationship between sex and the immune system have convinced Kovats that, while greater inclusion of women in studies has improved our knowledge base, current approaches to research often continue to ignore crucial information. “Whenever we take blood, we need to be measuring hormone levels,” she says. “We need to be asking women if they’ve undergone menopause, if they’re on hormone replacement therapy. Do they have ovaries?”
Without this information, she says, the data paint only part of the picture. And any conclusions drawn from that data will likewise remain incomplete.
Hiding in Plain Sight
At least for one disease area, that incomplete picture has been hiding in plain sight for years. “We’ve known for some time that most autoimmune diseases are heavily female,” says OMRF’s Dr. Hal Scofield, a physician-scientist who has studied the conditions for more than three decades.
In autoimmune disease, the body mistakenly turns its defenses against itself. Encompassing more than 80 known conditions, autoimmune diseases affect an estimated 25 million Americans, about 20 million of whom are women. For individual autoimmune illnesses, the statistics can be even more unbalanced: Lupus strikes women at a rate of about 9 to 1; in Sjögren’s disease, where the body destroys its moisture-producing glands, the ratio is more like 15 to 1.
Still, says Scofield, when he opened his lab at OMRF in the early 1990s, few scientists seemed interested in digging deeper into these sex disparities. A prevailing theory was that higher levels of hormones, especially during childbearing years, made women more prone to autoimmune diseases. Yet, says Scofield, “It was just considered an interesting question that wasn’t really studied.”
Women typically have two X chromosomes, while men usually carry one X and one Y. As the result of what he at first thought was a mix-up of samples, Scofield identified a male lupus patient who had an extra X chromosome, a condition known as Klinefelter’s syndrome. He and other OMRF researchers then decided to run genetic analyses of biological samples they’d gathered from almost 1,000 people with lupus. Only 200 or so were men, but among them, the researchers found five with Klinefelter’s. This led Scofield to a revelation of sorts.
“It turned out that men with Klinefelter’s syndrome had the same risk of lupus as women,” he says. So, at least for this particular autoimmune disease, “The primary risk factor is not whether you’re a man or a woman. It’s how many X chromosomes you have.”
Scofield’s research now centers on trying to tease out how these chromosomal differences set the stage for molecular and genetic changes that spur autoimmune diseases. He’s also curious about the role that sex hormones like estrogen may play. And here, the story ties back to the research of his OMRF colleague Kovats.
“In many ways, the female immune system works better than the male immune system,” Kovats says. Scientists have come to see autoimmunity as an overactive immune system, one that launches a protective volley against some sort of external trigger (perhaps a virus) and then continues that response against its own cells and organs. So, she says, autoimmunity may prove to be a sort of “trade-off,” the biological price that women pay for having a more vigilant immune system.
The long game, say both Kovats and Scofield, is to develop a fuller, more nuanced picture of human disease, one that takes into account the many factors associated with sex. That includes, says Scofield, variables that go beyond biology.
“Think of common diseases like hypertension, lung cancer and pancreatic cancer. All of them are much more common in men,” he says. “Some of that has got to be biologic differences. Some is not.” For example, he says, the sex differences associated with lung cancer have a clear environmental component: Men smoke more.
The goal of research going forward should be to identify as many of those components – behavioral, environmental, genetic, sex-linked – as possible. That way, clinicians can control for them and modulate their courses of treatment accordingly. In some cases, that may mean a specific drug that works better in one sex. In others, it may be a specific type of hormone replacement therapy tailored to a person’s unique biological profile.
The Longevity Paradox
For as long as statistics have been kept, women have outlived men. Part of that is linked to behavior: Men are more likely to die by suicide, in car accidents and as victims of violent crimes. Nevertheless, as people reach their 80s, 90s and beyond, a time when those variables should begin to fade into the statistical background, women’s survival advantage continues to grow.
According to Boston University’s New England Centenarian Study, of Americans who reach the age of 100, 85% are women. And of those who join the hyper-exclusive ranks of supercentenarians, those aged 110 or more, the female prevalence may rise to 90%. Still, the study’s leaders note that while women “far and away win the longevity marathon,” the men who make it to these advanced ages “are generally functionally better off and healthier.”
OMRF’s Stout acknowledges this seeming paradox. “Based on the scientific literature,” he says, “there’s a much higher probability of your child living longer if they’re female. But there’s also a stronger chance of a female having frailty over an age-matched male.”
Increasingly, researchers recognize that sex-specific biological mechanisms are helping drive these outcomes, says Stout. But what, exactly, are those mechanisms? And how much do they contribute relative to other factors?
“Those are things we just don’t know,” he says.
When it comes to sex differences in disease, there remain more questions than answers. But, driven in no small part by funders like the NIH, scientists now are focusing their microscopes on those questions.
At OMRF’s most recent scientific retreat, that research trend was evident.
The annual event brings together OMRF’s research staff for two days. However, due to the pandemic, the retreat went on a three-year hiatus from 2020 through 2022. When the event returned in 2023, a number of the featured presentations focused on sex as a biological variable.
“That was a huge difference,” says Scofield, who’s been attending the event for decades. Indeed, he can’t remember a single presentation by a colleague on the topic at the 2019 retreat. Or, for that matter, at any previous retreat.
Of course, it’s one thing to study a problem, another to find a solution. But you can’t get answers without asking questions. And at OMRF, that’s precisely what researchers are now doing.
—
Read more from the Winter/Spring 2024 issue of Findings
Road Music
Planting Seeds
Voices: Meg Salyer
Ask Dr. James: Does a lifetime of radiation from medical imaging pose risks to patients?
Pain Killer
Living Legacy
Data Nerd