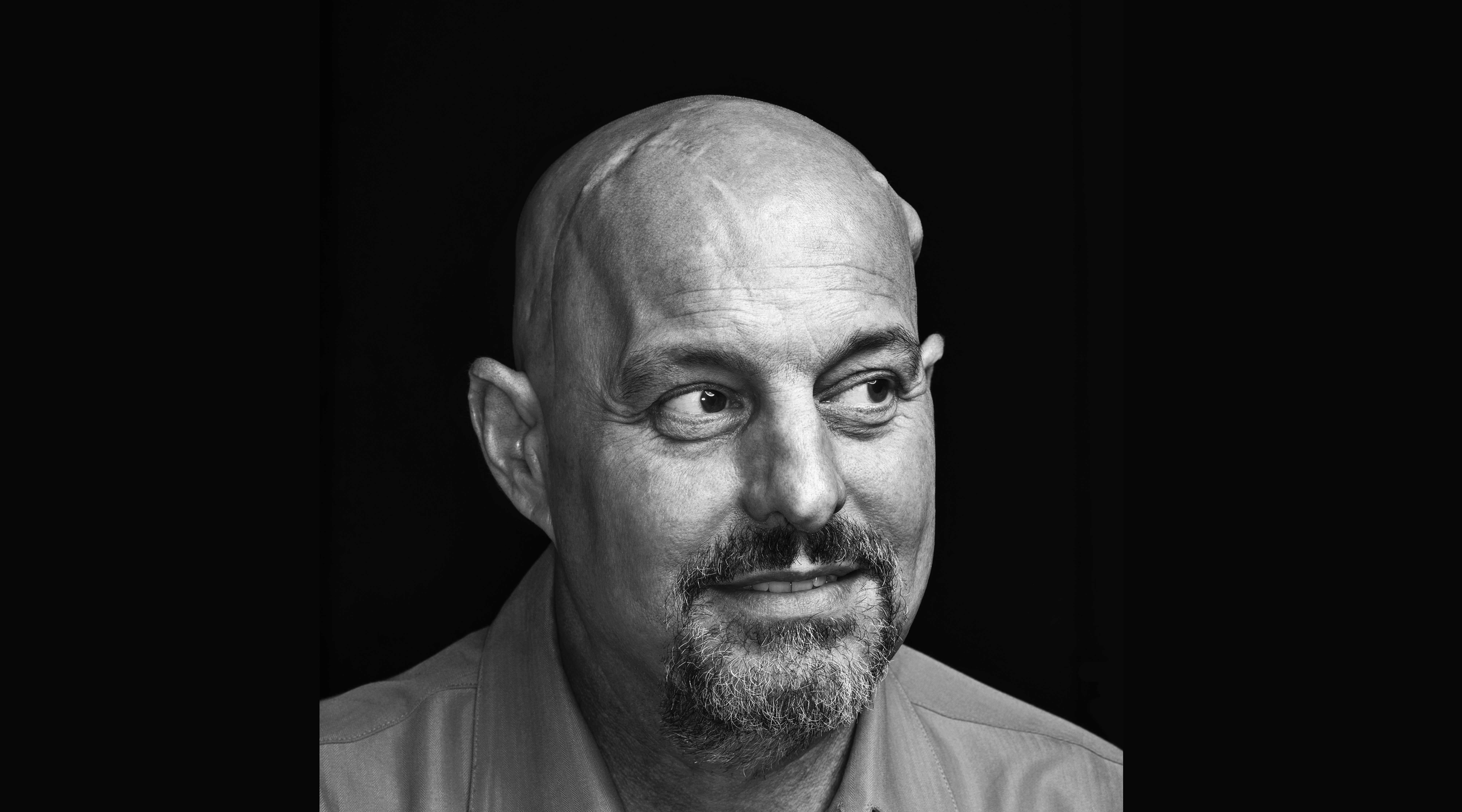
Doctors exhausted conventional treatments for Mike Schuster. Can an experimental OMRF drug stop his brain cancer?
***
In the summer of 2010, Mike and Teresa Schuster took their two boys to Mexico’s Yucatan Peninsula. The Schusters live in Norman, where Teresa is an administrative assistant in the University of Oklahoma’s Office of Student Affairs and Mike has worked in the restaurant and roofing industries. But whenever they have the chance to hit the road, they do. “Travel is our favorite thing to do together,” says Mike.
Mike rented a car in Mexico, as he wanted to bring Teresa and their sons, Parker and Connor, to sites off the well-worn tourist path. In the cities, Mike navigated narrow, traffic-choked roads, dodging pinballing buses and honking cars. “It was terrifying,” recalls Teresa. But the urban hurly-burly soon gave way to countryside, and the Schusters found their way to remote villages and Mayan ruins. It was near the remains of one ancient settlement that they discovered their first cenote.
The Yucatan is a flat, thick shelf of limestone. Beneath this layer of rock is a network of water-filled caves, all linked by subterranean rivers. When the roof of one of the caves collapses, it produces a sinkhole known as a cenote.
Because this particular cenote’s roof had only partially given way, from the earth’s surface, it looked like nothing more than a hole in the ground. But when the Schusters climbed down the hole on a wooden ladder, they found themselves in a massive underground chamber that had no floor—only a pool of water that stretched from wall to wall.
Mike made his way to the edge of a rocky outcropping and peered down. In the cave’s dim light, the liquid appeared black as pitch. There was no telling what might lurk beneath its surface, nor how deep it went.
Still, he hadn’t come all this way simply to look at the water.
Sometimes, he thought, you have to take a chance if you want to experience life in all of its richness. Sure, there are always risks. But without risk, there’s no reward.
So Mike took a deep breath. And then he jumped.
***
On the afternoon before Thanksgiving five years later, Mike was not thinking about cenotes or the Yucatan. The clock on his desk in Newscastle, Okla., where he worked as a consultant for a roofing company, said 1:00. Just finish up the numbers for this last job, he told himself, and you can call it quits for the holiday weekend.
He remembers studying the numerals that filled his computer screen. Then nothing.
He awakened gradually, finding his senses bit by bit. Voices swirled around him. A siren wailed nearby. He opened his eyes and saw he was in the back of an ambulance, atop a stretcher. You’ve had a seizure, someone told him.
This was a first. Mike, then 50, had never before had a seizure. As far as he could recall, everything had been normal until the moment he pitched out of his desk chair. No headache or dizziness. No warning of any kind.
At the hospital, the doctor ordered an MRI of Mike’s brain. When his physician tacked the film to a light box, Mike could see the white outline of his skull. Equally visible was a bright, oval-shaped spot on the right frontal lobe of his brain. About the size and shape of a kiwi, the brain tumor had formed just above his right eye.
***
“I’ve been healthy all my life,” Mike says. “No medical issues at all. I just couldn’t believe that this was happening.”
The doctor told Mike his tumor was a form of brain cancer. It has to come out immediately, the doctor said. He scheduled the surgery for the morning after Thanksgiving.
A brain tumor is an abnormal growth of cells in or close to the brain. Because the brain controls a multitude of bodily functions, tumors can have a dizzying array of effects, ranging from the seizure Mike experienced to impaired speech, comprehension, memory, vision, balance, judgment, hearing and reasoning. Tumors can also profoundly alter a person’s moods, personality and decision-making.
Brain tumors most commonly begin in other parts of the body and then spread to the brain. But in Mike’s case, the tumor originated in his brain. These growths, known as primary brain tumors, begin when normal cells acquire errors—mutations—in their DNA. The mutations cause cells to grow and divide at accelerated rates and to continue living when healthy cells would die. Over time, this results in a mass of abnormal cells, which forms a tumor.
Of the more than 120 types of brain and central nervous system tumors, Mike’s type, known as a glioblastoma, is the most aggressive. Senator Edward Kennedy died of glioblastoma, as did Beau Biden, son of former Vice President Joseph R. Biden, Jr. Senator John McCain was also recently diagnosed with this form of brain cancer.
Formed from the glue-like supportive tissue inside the brain, glioblastoma cells reproduce rapidly, fueled by the brain’s extensive network of blood vessels. The standard treatment regimen involves surgery to remove as much of the tumor as possible, followed by radiation and chemotherapy. Still, the tumor almost always grows back in a year, which typically triggers a second surgery.
Because they keep returning, glioblastomas are rarely cured, and the prognosis is poor. With treatment, the median survival—which means half of patients live longer, and half die sooner—is 12 to 18 months. Only one in 20 patients will survive five years.
***
For Thanksgiving, Mike opted out of the family celebration hosted by Teresa’s grandparents. “There were so many people in town, and I just didn’t think I could handle it.” Instead, he spent the day at home, watching black-and-white movies. Getting himself centered.
He happened across “The Long, Long Trailer,” an old Lucille Ball movie. In the film, Lucy and Desi Arnaz play newlyweds whose honeymoon trip runs predictably amok. Lucy gets frazzled, Desi gets angry, lots of things get broken.
Still, by the time the credits rolled, everything had turned out just fine.
The next morning, in a procedure that lasted six hours, surgeons removed as much of Mike’s tumor as they could. When they finished, they screwed in a titanium plate to replace the portion of his skull they had cut away. Then they closed the wavy incision that snaked across the top of his head with dozens of precise stitches.
When Mike regained consciousness, he was, understandably, “a bit woozy.” But the essential Mike, he soon discovered, remained unchanged. His faculties seemed unaffected.
On the right side of his head, a tube protruded from his incision, allowing the surgical site to drain. An I.V. dripped into his arm, and a half-dozen different monitors attached to his body tracked his heart rate, oxygen retention, blood pressure and assorted other vitals.
“I was hooked up to so much stuff that I could hardly move,” he says. “I had to call for help just to go to the bathroom.”
His surgeon explained that he’d succeeded in excising most of the tumor. But, he said, like most glioblastomas, this one had “tentacles.” Tiny arms of the tumor had grown into surrounding brain tissue and could not be removed.
Just take it easy for now, said the surgeon. You need to get your strength back. Then we’ll focus on getting the cancer that’s still inside you.
***
In a few days, Mike’s doctor removed the tube from his head—“He yanked it out like he was pulling off a Band-Aid”—and released him from the hospital. At home, Teresa kept a close eye on her husband, watching for any changes. But other than fatigue, which took hold quickly, she saw the same person she’d been married to for more than two decades.
Gregarious and social by nature, Mike wanted to get back out in the world. He liked seeing and interacting with people. But he was self-conscious about the scar on his head, which, he says, looked like “the stitching on a baseball.”
When Teresa would take him out, Mike would immediately spot someone he was sure he knew. “I’d say, ‘Hey, how are you doin’? I haven’t seen you in awhile!” After a brief, awkward conversation, he’d discover that, indeed, he hadn’t seen that person recently. Or ever. Each time, the “friend” would turn out to be a perfect stranger.
One doctor didn’t know what to make of the phenomenon. Another had read of such surgery-induced déjà vu. But with Mike’s speech and memory fully intact, they didn’t worry much about it. And within a week or two, Mike stopped mistaking people he’d never met for long-lost pals.
Life, though, didn’t quite return to normal. Mike was unable to go back to work. He did a little consulting, writing a computer program for one company. But, otherwise, he found it tough to maintain focus.
Everyone, it seemed, wanted to hear his story. How did it happen? What were the signs? How are you feeling?
Mike appreciated the concern. But he didn’t want to be the guy with cancer forever talking about his condition. “Sometimes, I’d tell Teresa I just couldn’t handle talking about it anymore.”
In December, he traveled to Colorado for his son’s college graduation. The journey and extended absence from home was, he says, “tough” on his body. But he was happy to be regaining some sense of normalcy, to be doing the two things he cherished most in life: traveling and spending time with his family.
As he watched his son receive his diploma, Mike thought, this is a moment I wouldn’t have wanted to miss for anything. And he hadn’t.
Once he’d recovered sufficiently from surgery, he began a follow-up treatment regimen at the Stephenson Cancer Center at the University of Oklahoma. For six weeks, he’d travel each weekday to Oklahoma City, where doctors would focus a powerful beam of radiation into his skull. Even though Mike couldn’t feel the electromagnetic waves pulsing through his brain, “you could smell it,” he says. He also started chemotherapy, taking a pill called temozolomide. Together, the treatments were intended to kill the tumor cells that remained in the fissures of his brain.
“If you leave even a single cancer cell in the brain, it can regrow,” says Dr. James Battiste, the neuro-oncologist who oversees Mike’s care at Stephenson. “The brain is fertile soil for these tumors. That’s why chemo and other therapies are so important.”
Radiation and chemotherapy, though, are blunt instruments, killing much more than cancerous tumor cells. Mike’s hair, which had begun to grow back following the surgery, fell out. Ditto with his right eyebrow.
Still, Mike tolerated the therapy well. He maintained his appetite throughout, managing any nausea with medication. By the end of radiation—doctors limited his treatment to six weeks for fear of triggering a secondary cancer—he even decided he liked the Bruce Willis look and continued to shave his head. (He also kept a goatee, which he’d grown during radiation treatments “to have a little hair on my face.”)
He stayed on temozolomide. As the months piled up, he became increasingly optimistic; periodic MRIs showed that, while pockets of tumor cells still lurked in his brain, they weren’t spreading. By late November, brain scans continued to show no new growth.
Mike was elated. The previous year, he’d spent Thanksgiving grappling with an impending surgery for a lethal brain tumor. The 2016 holiday couldn’t have been more different. “I was telling everybody I didn’t have cancer. Teresa would say the word, and I’d say, ‘no.’” As far as Mike was concerned, he’d beaten the disease.
Four weeks later, an MRI of his brain revealed a new tumor.
***
Awake surgery was pioneered decades ago in epilepsy patients; anesthesiologists would keep patients alert enough to ensure surgeons were destroying the brain tissue that triggered seizures. With the advent of sophisticated brain-mapping technology and anesthetics, use of the technique has blossomed in recent years. It’s become the go-to surgery for many types of brain tumors, especially ones like Mike’s, which was perilously close to tissue that controls motor skills and other sensory abilities.
The advantage of keeping patients awake, says Battiste, is that surgeons can remove more of the tumor and parts of the associated tentacles without the risk of added damage to the brain. And because neurons in the brain don’t have any pain receptors, so long as the scalp is numbed properly, patients don’t feel anything that surgeons are doing in the brain itself.
In early January of this year, after administering an anesthetic, Mike’s surgeons inserted screws in his skull and mounted them to a metal halo to immobilize his head. “I could hear the buzz as they drilled holes in my head,” says Mike, “but I couldn’t feel anything.”
Tumor fragments had attached to his skull, and the surgeons removed them using a chisel. Again, there was no pain, but each blow of the surgeon’s hammer resonated in Mike’s jaw.
As the doctors worked, a physical therapist kept Mike engaged by having him move pegs around a peg board. At intervals, she’d also ask him to perform other tasks.
“Recite your ABCs,” she’d instruct him. When Mike would dutifully comply, she’d say, “Now count backward from 21.” The exercises, which also included seemingly straightforward tasks like touching his fingers together, were more than mere busy work. Mike’s steady stream of responses served as a sort of cartographic warning system to the surgeons; when he displayed any sort of difficulty, it would alert the doctors they were probing dangerously close to a region of the brain that controls language or other sensory abilities. Even a nick in such a no-go zone could leave Mike unable to speak or understand language for the rest of his life.
After nearly half a day, the surgeons once again secured the titanium plate that, for the past 14 months, had replaced what had previously been skull. Once more, they had removed the principal tumor. They’d also scraped and dug out many minuscule fragments that had grown in other parts of his brain.
He also had a new addition on the left side of his scalp: a grape-sized bump where doctors had placed a valve under his skin. Connected to a pair of tubes, this shunt system relieved pressure on his brain by draining excess fluid into his stomach.
Late that night, Mike underwent a post-surgical MRI. His doctors wanted to see if any portions of the main tumor had eluded their scalpels. “Waiting for those results was tough,” says Mike. Happily, the brain scan showed that the doctors had succeeded in removing all of the primary tumor.
Still, many glioblastoma tentacles had escaped their reach, remaining lodged in his brain.
Mike spent five days in recovery. Despite the ostensibly successful surgery, he found his spirits flagging. “I’d thought that I had it beat. And now, I felt like I was starting all over again.”
He knew those tentacles were, in essence, seeds that could sprout another full-blown tumor in a matter of weeks. They’d already done it once. What was to stop them from doing so again? And now, having reached his body’s limits for radiation and chemotherapy, he could no longer rely on them to keep his cancer in check.
Mike told Battiste he was willing to try anything to beat back the glioblastoma. In particular, he’d read about clinical trials of experimental medications. Was there one of these that might help him?
Stephenson has more than 200 different clinical trials for new cancer drugs underway. Battiste, in fact, was leading a trial that, he says, “just seemed suited for Mike.” The trial was designed to test an investigational medication for glioblastoma. Coincidentally, that drug had been born just down the block from Stephenson—in the labs of OMRF.
***
The experimental medication known as OKN-007 was discovered by OMRF’s Dr. Robert Floyd. Originally conceived of as a treatment for stroke, the compound attracted the interest of pharmaceutical giant AstraZeneca, which spent years refining and testing the drug. The medication successfully completed the first two phases of human clinical trials, but in the final stage—which involved thousands of stroke patients around the world—it failed to show efficacy. So the company mothballed the drug.
Floyd, though, wasn’t prepared to give up on OKN-007. In previous pre-clinical experiments, the compound had shown a significant amount of anti-cancer activity. Dr. Rheal Towner, a colleague at OMRF, had been studying the use of similar compounds as potential cancer therapeutics. For those experiments, Towner had developed a method of implanting and growing glioblastoma tumors in rodents. Based on that work, Towner decided to administer the drug to one of his glioblastoma rats. Within weeks, 90 percent of the animal’s tumor melted away.
“We were amazed,” says Towner. He repeated the experiment in several different rodent glioblastoma “models,” and each time, tumors shrank and survival rates increased. “The compound,” says Towner, “was working.”
Even three months later, in rodents whose brains had once been riddled with cancer, the scientists found no evidence of recurrence. Testing showed the compound dramatically decreased cell proliferation (spread) and angiogenesis (formation of new blood vessels), and it turned on apoptosis, the process of removing damaged cells so they can’t become cancerous. “Those are the three major factors needed in a cancer drug,” says Towner. “This compound seemed to do all of them.”
Unlike most experimental drugs, thanks to its clinical trials, OKN-007 had an extensive, well-documented history of how it behaved in humans. Although it had not been found to be effective in remedying strokes, it hadn’t shown any dangers or side effects. With that safety data in hand, plus the promising results of Towner’s rodent experiments, the FDA gave OMRF the green light to begin testing OKN-007 in glioblastoma patients.
***
In July, Mike sat in an overstuffed chair in the infusion suite at Stephenson Cancer Center. When a nurse approached, he unbuttoned his Hawaiian shirt, and she felt around until she found a raised area on the right side of Mike’s chest. This was the end of a port his doctors had inserted to serve as a sort of artificial vein.
After the nurse hooked an I.V. bag to the port, Mike re-buttoned his shirt and reclined in the chair. For the next hour, clear liquid—OKN-007—dripped through the tubing into Mike’s chest, where it was distributed through a large vein near his heart into his bloodstream. From his circulating blood, it passed through a semipermeable membrane into his cerebrospinal fluid, which then delivered the medication to his brain. There, it provided a sort of chemical marinade for the remaining tumor cells, immersing them in a powerful bath of anti-cancer agents that would prevent growth and spreading.
At least that’s what Towner and Battiste hoped was happening. With this clinical trial, they’ll find out if this is, indeed, the case.
Clinical trials are the FDA’s process for evaluating new drugs. For safety purposes, testing starts with small groups of patients to find out whether a drug causes any harm. In later phases, researchers learn more about the compound’s risks and benefits.
OKN-007 is now in the first phase of its clinical trial, which primarily focuses on the drug’s safety. “We look at potential side effects and learn what dosage levels might cause problems,” says Battiste. But they’re also examining efficacy, studying each MRI to determine “How is the brain doing?”
Trials represent a significant time commitment for patients like Mike, who comes to Stephenson up to three times a week for infusions. He also receives regular blood work and MRIs, which means his visits to the cancer center can last for up to five hours. “You can’t work a regular job” around this regimen, Mike says. Still, he says the experience is “almost like a spa day. Everybody at Stephenson is so nice. They feed you. And you even watch TV while you get your infusion.”
So far, Battiste is cautiously optimistic about the performance of OKN-007 in his patients. “We’ve gone to the highest dosage levels the FDA would allow, and we haven’t seen any negative effects from the drug.” And while evaluating the medication’s effectiveness in controlling the regrowth of tumors is only a secondary endpoint at the moment—later trial stages focus on efficacy—“it’s helpful to see things looking good” on this front, too, he says.
Given the relatively rare incidence of glioblastoma, which strikes 2 to 3 out of every 100,000 people, recruiting study participants has proven slow. Although the trial opened four years ago, Mike is one of only about a dozen patients who have taken part. With such small numbers, Battiste says, determining the statistical significance of results can be challenging.
What comes next will be up to Oblato, a Korean biotechnology company that acquired the rights to OKN-007 last year. One path would be to petition the FDA to move to a phase II trial. This would shift the focus of testing from safety to effectiveness and involve more patients, likely at multiple clinical centers (currently, Stephenson is the only trial site).
Another approach, says Battiste, would be to seek FDA approval to increase dosage levels. “In oncology, the thinking is that if one dose is good, a higher dose must be great. And at the current dosage levels, we haven’t seen any side effects.” Or the company could initiate a new phase I trial using an oral formulation of the drug. “A pill would make it more convenient for patients,” increasing usage. Plus, it would provide a more constant level of medication in the body. “If you soak the brain in something, it can be more effective.”
***
On August 8, Mike celebrated his 52nd birthday. A couple of weeks earlier, he’d also marked another significant milestone: at 20 months and counting since his diagnosis, Mike had exceeded the life expectancy for the average person with glioblastoma.
When he sees other patients with brain tumors, he says, they appear thin and frail. Mike, on the other hand, has added 15 pounds since he began OKN-007 infusions. “So far, I’ve had no side effects at all,” he says. “I’m never tired, never feel sick.”
Mike can’t say enough good things about the care he’s received at Stephenson. “Everybody has been so great. It’s the place to go if you’re unfortunate enough to get cancer.”
His faith, he says, has also buoyed him throughout this process. “The power of prayer and my faith in God have helped sustain us.”
He’s grown strong enough to drive himself to appointments and to take Teresa out to dinner. “I’ve been able to get back to the gym and am doing some yard work. I feel really good.” Best of all, he says, “My MRIs are looking good.”
He’s even begun to think about travel again. If all continues to go as planned, once he finishes the phase I trial in the fall, he’d like to take his family to Cuba.
Of course, neither Mike nor his doctors can know for sure if the drug is responsible for keeping his cancer at bay. Nor can they say if, or when, the disease might recur. “I can’t worry about stuff,” says Mike, “that’s out of my control.”
Still, he feels certain he made the right decision when he opted to participate in the clinical trial. Yes, there were—are—perils to receiving treatment with an experimental drug. But, just like that time he took the plunge into the cenote in the Yucatan, without risk, there was no possibility of reward.
Mike believes he’s receiving that reward with each new day. “Let’s just say I’ve been very blessed. It’s pretty cool how this stuff is working.”
Right about then, a monitor beeps. Mike’s infusion treatment for the day is finished. A nurse arrives and detaches the drip line. Mike buttons his shirt.
Telling your story is fine when you’re hooked to an I.V. and your only other option is to watch TV. But now Mike has a choice to make: he can either keep talking about his cancer, or he can go and live his life.
Mike gives his interviewer a hug. Then he picks up his keys and heads for the door.