Long before he ever set foot in a research laboratory, Dr. Joel Guthridge understood what it meant to be team player.
In the late 1970s and early 1980s, he strapped on pads as an offensive and defensive tackle on his Iowa high school football team. Listen to your coach. Practice hard. Come game day, you do your job—whether that means throwing a touchdown pass or, for Guthridge, battling in the trenches so your quarterback can make that winning toss.
But whatever that job is, you bring your A game.
Guthridge later transitioned from player to coach, using that team-first mindset as a mentor, judge and state tournament organizer for high school robotics competitions. “In robotics, everyone had a set of skills that had to be managed and focused toward a common goal,” he says. “‘Gracious professionalism’ was our motto. Work and compete furiously, but graciously. In other words, work to better everyone, even your competition, because you could be competitors in one match and teammates in another.”
Although Guthridge didn’t know it at the time, those experiences would help prepare him for perhaps the biggest challenge of his scientific career: creating a dedicated, high-volume clinical testing laboratory for Covid-19.
—
On New Year’s Eve 2019, Chinese health authorities confirmed they were monitoring a new and unknown virus. Within days, they announced the first death from the novel coronavirus in the Wuhan Province of central China. Japan, South Korea and Thailand soon reported cases, and in late January, a Washington state man exhibited symptoms after returning home from a trip to Wuhan.
The U.S. reported its first death on Feb. 29, and by mid-March, many Oklahoma businesses, including OMRF, issued work-from-home orders to employees. Schools closed, and restaurants and shops went dark as citizens hunkered down.
Like most Americans, Guthridge followed news on the virus known as SARS-CoV-2. A specialist in genetics and bioinformatics, he’d spent two decades studying lupus and other autoimmune diseases at OMRF. With the pandemic, Guthridge saw a way to help.
Scientists like Guthridge have used polymerase chain reaction, or PCR, testing equipment in their laboratories for years. First developed in 1984, the technology is the cornerstone for much of the genetic testing available today. With it, researchers can take a tiny DNA sample and amplify it millions of times, enabling them to identify even minuscule amounts of infectious agents.
PCR testing revolutionized forensic science and also allowed researchers to gather vast amounts of data from small quantities of sample materials. A special technique called reverse transcription PCR, or RT-PCR, added further power, enabling researchers to detect the presence of even a single particle of a virus deep inside a sample.
Guthridge had employed the process to study autoimmune diseases like lupus, multiple sclerosis and Sjögren’s syndrome. Now, in the pandemic, he envisioned a new use.
“We knew we had technology that could be used, but it needed some adaptation to do large-scale clinical testing,” says Guthridge. “We realized it was time to offer our assistance in the testing effort.”
When the pandemic hit Oklahoma, the state had only minimal testing options available. In most labs with standard equipment on hand, technicians could only complete a few dozen tests per day. So, they limited testing to those exhibiting virus symptoms, those with a known exposure to the virus, healthcare professionals and first responders. As cases multiplied, health authorities realized things had to change.
“This was a major unmet need,” says OMRF Vice President of Clinical Affairs Dr. Judith James, who worked with Guthridge to formulate a plan. “Everyone recognized we had to have more testing.”
Guthridge also started talking with Dr. Graham Wiley. As director of OMRF’s next-generation DNA sequencing facility, Wiley knew what it took to perform genetic testing on a large scale. Like Guthridge, he believed that scientists could employ “high-throughput” methods like RT-PCR to significantly increase testing capacity. “Talking about doing thousands of samples at a time didn’t sound scary to me,” Wiley says.
Guthridge, James and Wiley compiled spreadsheets with the equipment and supplies they’d need to process clinical tests. With those in hand, Guthridge and James reached out to the OU Health Sciences Center.
OMRF and OUHSC are neighbors; 13th Street separates the two campuses in northeast Oklahoma City. And while they’re frequent collaborators, the two institutions can find themselves as competitors for grant dollars and philanthropic funding.
Here, though, any sense of rivalry disappeared. “We shared a single goal: to help Oklahomans in an unprecedented time of medical need,” says OMRF President Dr. Stephen Prescott.
At OUHSC, Guthridge and James reached out to Dr. Michael Talbert, Lloyd E. Rader Professor and Chair of the Department of Pathology, to help lead the effort. They also enlisted Dr. Rufei Lu, a third-year pathology resident who’d trained at both institutions.

“Rufei was our secret weapon,” says James, who heads OMRF’s Arthritis & Clinical Immunology Research Program and also holds the Lou C. Kerr Endowed Chair of Biomedical Research at the foundation. “He’s a computer whiz with a degree in chemical engineering. Plus, knowing OMRF’s strengths helped make the collaboration possible.”
Troubleshooting and brainstorming sessions helped Guthridge and his colleagues draw up a plan. They talked immunology and virology, but also engineering, robotics and logistics. Each team member brought unique skills. “None of us could tackle this challenge alone,” says Guthridge. He acted as strategist, facilitator and organizer, a coaching role long familiar to him.
The team conferred with the Oklahoma State Department of Health and the Oklahoma City-County Health Department to organize the test flow. Both had already established drive-through testing centers around the state. The new OU Medicine lab would need to develop a system to collect the samples for processing and return the results to patients and healthcare providers. The faster the turnaround, the better to isolate and treat infected individuals—and to identify potential viral hotspots before they got out of hand.
Talbert, who also serves as chief of pathology and laboratory director for OU Medicine, identified empty space that could serve as the testing lab’s home. Under his guidance, an OU Medicine facilities crew renovated the space to accommodate the personnel and specialized equipment the effort would require. “We made fast changes,” Talbert says. “We even put up a wall in one day.”
Then Guthridge turned to OMRF staff for the next part of the process: moving essential pieces of scientific equipment from the foundation to OU Medicine.
The centerpiece of the effort would be an RT-PCR testing system called the Fluidigm Biomark HD. Purchased by OMRF for $300,000, the Biomark would provide key advantages over testing platforms other labs were utilizing.
In the pandemic, labs were consuming unprecedented amounts of reagents, the chemicals needed to process tests. As a result, supply chains for reagents were drying up.
The Fluidigm system, though, relies on different reagents from standard PCR machines. And it employs a technology known as “microfluidics,” minimizing the amounts of those reagents required to run tests. The Biomark also possesses the ability to process multiple samples at once, meaning that it holds the potential to deliver many times more results on a daily basis than a standard testing system.
“Think about microfluidics like a computer chip,” says Mark Lynch of Fluidigm. “Back in the day, computer chips were massive. You couldn’t have a laptop, only a desktop PC. What we’ve been able to do is take a laborious, time-consuming, labor-intensive process and automate it with a microfluidic chip.”
Led by Guthridge, Wiley and Sean Turner, a lab manager at OMRF, the foundation’s biomed staff powered down the equipment needed for the testing lab: the Biomark, another PCR processor, and other machines that would assist in the process. They swaddled everything in bubble wrap, and then—along with carts full of reagents, lab supplies and a new $35,000 robot OMRF purchased to accelerate the testing process—moved it to OU Medicine.
At OU, though, the team faced a challenge much greater than simply unpacking the equipment and plugging it back in. OMRF’s Guthridge and his colleagues had used the Biomark to process and analyze biological samples donated by patients suffering from autoimmune diseases. Now, they aimed to transform it into the backbone of a high-throughput coronavirus testing lab that would run thousands of tests to diagnose the coronavirus each week.
“It was a completely novel idea to use the equipment this way,” says Talbert, who oversees testing operations at OU that generate a total of approximately 5 million results each year. “No one had ever done this.”
That meant reconfiguring and reprogramming equipment for its new use, then running batches of validation tests to ensure the results they produced were accurate. When data didn’t pan out—as measured by Guthridge’s exacting standards—the team readjusted the machines and retested. Again and again and again.
“In medical testing, you have to prove you can do it right, over and over.” Wiley says. “Your mindset has to be methodical and thorough.”

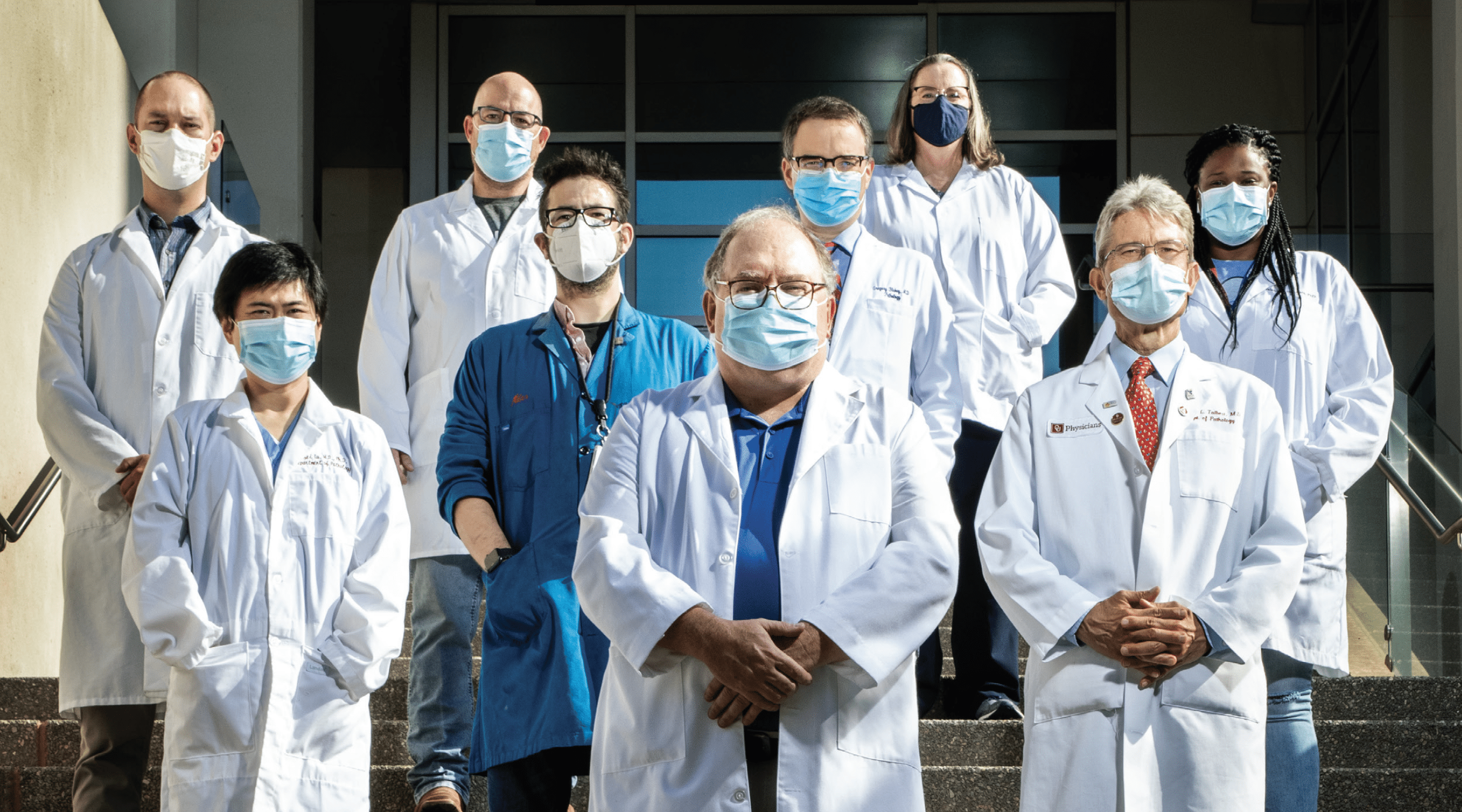
For weeks, the team lived this Groundhog Day-like existence, routinely pulling shifts of 12 hours or more. “They worked night and day, 7 days a week, and often didn’t even know what day it was,” says James. OU Medicine provided pathologists and staff for the new facility, and the team—which included OMRF’s Guthridge, Wiley and Turner, plus Drs. Valerie Lewis, Miles Smith and Carla Guthridge (Joel’s wife) and OU’s Drs. Rufei Lu, Cindy McCloskey, Ken Jones and Greg Blakey, as well as Sarah Jonas-Bond, Tyler Shadid, Phil O’Neill, Leena Suppiah and Andrew Gross—trained them to operate the equipment.
Smith, a virologist, teamed with Lu and McCloskey, pathologists, to do much of “the heavy lifting in the viral lab,” says Joel Guthridge. “They drove the science at many steps of the process.”
As cases in Oklahoma kept mushrooming, the group felt increasing pressure to get the lab up and running. Still, even a single false negative could send an infectious person back out into the world, triggering a cluster of new cases. They had to get this right.
Wiley formulated a mantra of sorts that summed up the team’s ethos: “Move fast, but don’t be rushed.”
—
While the team plowed ahead, across the street, OMRF remained in a state of suspended animation. Like many businesses, the foundation drastically altered operations with the arrival of the coronavirus. In mid-March, OMRF sent most of its staff home to work virtually until cases in the state subsided. For the next two months, the foundation operated in what came to be known as “skeleton crew” mode, with only a handful of clinical staff and other personnel onsite.
Against this backdrop, few would have faulted employees who voiced a reluctance to join the effort to set up the testing lab. Especially because—in the midst of a life-threatening pandemic—the very nature of the work prevented social distancing.
“To move equipment, two people had to lift it together,” Turner says. “We put protective gear on, always wore gloves, masks and disposable lab coats and kept hand sanitizer everywhere. We just tried our best.” Still, he says, “If you’re teaching someone else how to do something, they can’t be six feet away. They need to see what you’re doing.”
Nevertheless, the team members didn’t flinch.
“On a personal level, I felt like if I could help, I should,” Turner says. “I was honored to be asked.”
For Wiley, the decision to participate was really no decision at all. “I’m dedicated to OMRF’s mission to help people live longer, healthier lives,” he says. “So, when the call came to help, I stepped up.”
—
Until recently, if a manufacturer wanted to utilize a novel clinical testing method, it first had to receive formal approval from the Food and Drug Administration. Scientists prepared reams of documentation demonstrating the accuracy of the test, and the FDA typically took almost a year to complete its review process. Even a designation of Priority Review, the fastest track available, only guaranteed the agency would render a decision within six months of submission.
Then came the coronavirus.
In February, the FDA created an Emergency Use Approval process for Covid-19 tests. This expedited track allows the release of novel Covid-19 tests—like the one Guthridge had devised—in just a fraction of that time.

On June 30, the OU-OMRF team filed its application with the FDA to launch the new testing operation. “We had to submit quite a bit of proof that the test actually works as we describe it,” says Talbert. “In fact, we went beyond what they wanted.”
In the wake of the filing, the team continued to make refinements. “Normally, we’d have about six months to prepare the lab, so there were issues we still needed to work out,” Talbert says. Those included hiring and training additional laboratory personnel and, under the guidance of Carla Guthridge, integrating robotics into the process. Rather than requiring a pair of technicians to perform certain tasks, he says, “Now we only need one. It’s a wonderful thing.”
Although Talbert described the early days as “training mode,” the operation continues to ramp up. Each day, couriers deliver samples collected at OU Medicine facilities and at “swab pods” in Oklahoma City, Tulsa and Norman. Technicians then prepare and load batches of samples, up to 186 at a time, into the Biomark, where each run takes about six hours.
During that time, says Guthridge, the machine tests each sample five times, which ensures accuracy. And because the Biomark utilizes RT-PCR technology, it has a high rate of “sensitivity,” detecting infections other commercially available tests—especially the ones that deliver rapid results—can miss.
Most samples arrive in the afternoon. In a time when testing backlogs often force patients to wait a week or more to learn whether they have Covid-19, the lab typically reports results the following day. Sometimes, they’re able to deliver results that same day.
Still, the team is not resting on its laurels. While continuing to fine-tune methods and add staff, Guthridge, James and Talbert are also looking for ways to supercharge the number of samples they can process in a day. Specifically, they’re working on a concept called pooling, which would enable them to run four samples in the testing “wells” that currently hold one specimen. This change could quadruple the lab’s daily testing capacity—without using any additional reagents.
In addition, the group is investigating the use of saliva samples instead of mucus to test. If successful, this could substitute a simple spit-in-a-cup for the current nasopharyngeal swab, an uncomfortable process subjects have described as akin to “getting poked in the brain.”

Despite the fact that the collaboration arose in response to an unparalleled health crisis, Talbert says he can’t help but describe the process of working with his OMRF neighbors as “amazing” and “fun.” He’s also got one eye to the horizon, hoping to find new projects that can benefit from their collective talents. There is, he says, “so much expertise to tap at OMRF.”
James heaps praise on each member of the team and the respective institutions—OUHSC, OU Medicine, OMRF—that have made the effort possible. But, she says, others deserve credit as well.
“Our donors don’t think when they’re giving $20 or $40 in memory of a loved one that it’s going to support cutting-edge science not done anywhere else in the world,” says James. “However, without that kind of ongoing philantrophic support, this new testing facility wouldn’t exist.”
Like James, Guthridge is quick to credit a host of people for getting the lab up and running. “Please make sure to mention the work the biomed shop did in moving and recalibrating the equipment,” he says. “And don’t forget purchasing and accounting. They helped us get supplies in an environment where that was far from easy.”
He keeps going, rattling off names and singing their virtues. Not once, though, does he mention himself.
Because, of course, there is no I in team. Every good coach knows that.