When a fresh wound occurs, cells rush to produce collagen, which aids healing. But sometimes this process goes awry, resulting in one of two extremes: insufficient healing or excessive scar tissue.
Thanks to a recent discovery at the Oklahoma Medical Research Foundation, researchers now have a better grasp on the cause.
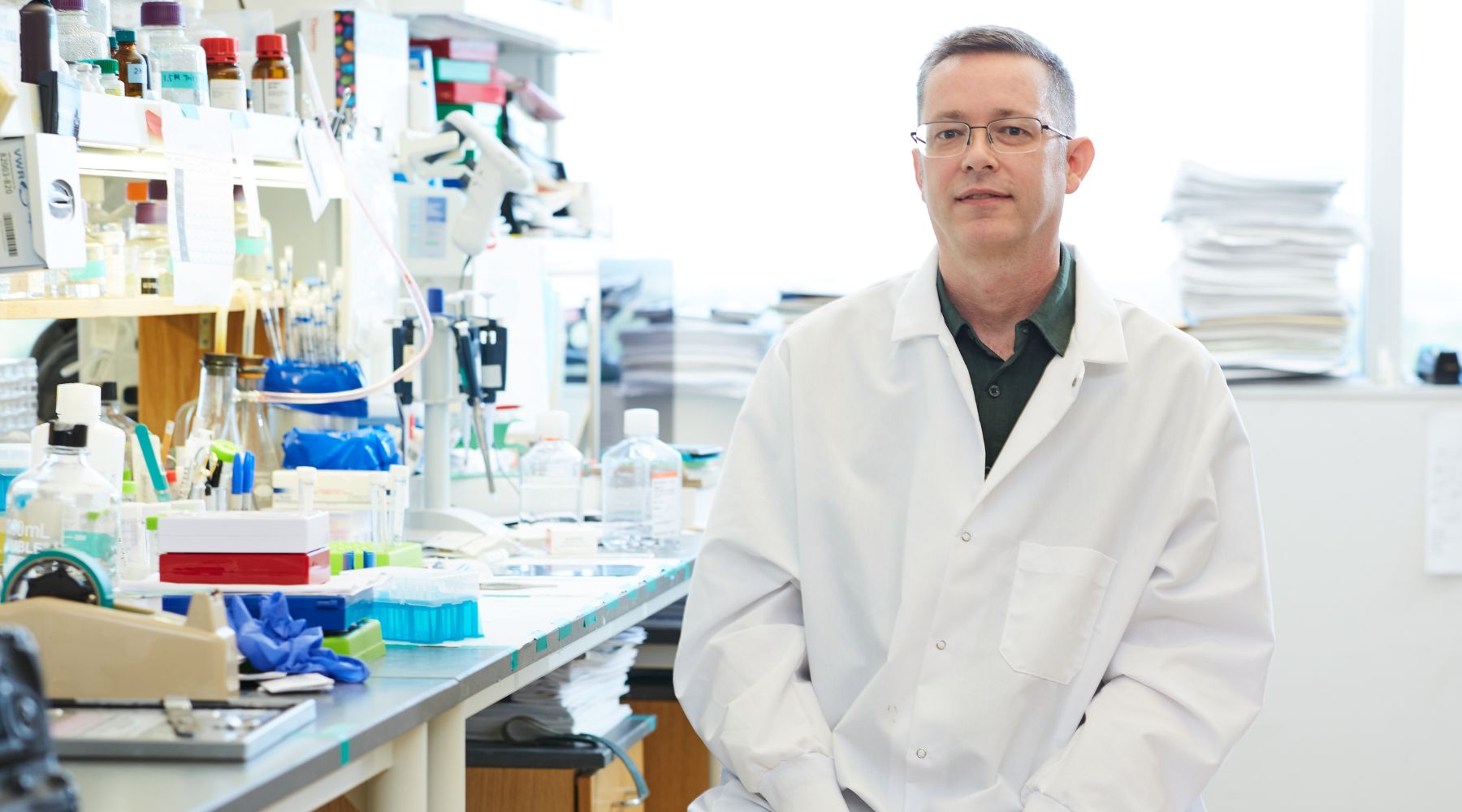
“It’s a delicate balance,” said OMRF scientist Lorin Olson, Ph.D., who led the study published this month in the journal Cell Reports. “Everything must work just right for proper wound healing to take place.”
Olson’s lab focused on a protein signal called platelet-derived growth factor (PDGF) and cells called fibroblasts, which create collagen to form scar tissue. Several days later, these cells morph into a different cell type called myofibroblasts, which pull the wound’s edges together, essentially closing it.
Working with researchers from the University of Oklahoma Health Sciences Center, Olson’s team discovered that PDGF controls this transition from one cell type into another and that optimal healing requires precise amounts of the protein signal.
“This paper focuses on wounds in the skin, but the same principles apply to injuries in other tissue or organs,” Olson said, “because in every injury, cells respond by migrating toward the damage.”
Too much PDGF results in wounds full of fibroblasts but no myofibroblasts, causing excessive scar tissue. In contrast, without sufficient PDGF, there aren’t enough fibroblasts to create collagen, and wounds fester.
Those chronic wounds cause significant medical and financial issues for millions of Americans. One common example is in people with diabetes. Poor circulation and nerve damage caused by the disease can lead to chronic foot ulcers, potentially requiring amputation. A 2018 University of Southern California analysis found that chronic wound treatment accounted for up to $96.8 billion in annual Medicare costs.
“Wound healing happens so routinely that we tend to take it for granted,” said Lijun Xia, M.D., Ph.D., chair of OMRF’s Cardiovascular Biology Research Program. “Dr. Olson has dedicated his career to better understanding the inner workings of this complex process. His discovery gets us closer to solutions for cases where a wound refuses to heal properly.”
Olson has taken these findings to delve into the cause of keloids – thick, often permanent, raised scars that most frequently form on the earlobes, shoulders, chest and cheeks of people of African and Asian descent. However, he said this discovery has far broader relevance.
“We’re studying PDGF signaling in conditions like atherosclerosis, where deadly plaque builds up in arteries, as well as cancer,” Olson said. “So if we better understand how it works, we can apply that knowledge to many other health conditions.”
Olson’s research is supported by National Institutes of Health grants R01-AR070235 and R01-AR073828, the Oklahoma Center for Adult Stem Cell Research, a program of TSET, and the Presbyterian Health Foundation.