It may sound like the set-up to an old joke. But for Judith James, the question of how to extract venom from a fanged spider roughly the size of a tea saucer was no laughing matter.
In zoology class at Oklahoma Baptist University, each student received an animal to study and care for throughout the semester. James, then a sophomore, knew her professor would not let his star pupil take the easy road; there’d be no cute and cuddly rabbits or hamsters for her.
“I assumed that because I hated snakes, he’d give me one,” she says. So she tried a little misdirection, delivering an Oscar-worthy display of feigned serpentine affection. “I spent three days holding snakes, even wrapping them around my neck.” The ploy worked—sort of. On D-day, James learned she’d spend the semester not as a would-be herpetologist but, rather, ministering to a group (technically, a wisp) of tarantulas. “They were,” she recalls with a slight shiver, “the biggest, hairiest spiders I’d ever seen.”
Most of her classmates came up with projects that analyzed their animals’ behaviors. They looked at things like whether mice were more active in day or night and how temperatures affect the activity levels of fish. But James decided she wanted to, in her words, “do something chemistry-ish.” She’d analyze her spiders’ venom, which can paralyze prey like insects and frogs. But how, exactly, do you get the fluid out?
After some research, she identified a professor at Oklahoma State University who worked with Brachypelma, as the furry arachnids are scientifically known. Come to my lab, he told her, and I’ll show you all you need to know. So she herded her eight-legged charges into a makeup case, packed it into her Pontiac Firebird, and headed an hour north on Highway 177 from Shawnee to Stillwater.
There, in a session that was part Addams Family, part CSI, James learned that step one in milking spiders is to put the animals to sleep. She accomplished this by placing them in shoebox-sized plastic cages, then adding dry ice and ether. Once the tarantulas lost consciousness due to the fumes, James would lay them on their backs in hollowed-out sponges. After securing each of their legs with Velcro strips (repurposed from kids’ sneakers), she’d apply a small electrical current at the base of the spiders’ fangs. And, voilà, out dripped the venom, which she’d catch in a capillary tube.
James had hoped to find components of the venom that stimulated changes in the neurons. Unfortunately, her grand plan didn’t quite pan out. “The venom pretty much killed everything.” Still, what she now describes as “an epic fail” did have its upsides.
First, no spider ever bit her. And when she recounted her tarantula tale in an interview for OMRF’s Sir Alexander Fleming Scholar Program, which had rejected her on two previous occasions, she was admitted. That brought her in the summer of 1988 to OMRF’s labs, where she’d spend two months. Or so she thought.
Because, you see, once James came to OMRF, she never left. Within days of her arrival, she’d already started down the road that would ultimately lead her to become one of the world’s pre-eminent lupus researchers.
Like so much of James’ life, the path she chose and the resulting outcomes were at once wholly unexpected and completely predictable.
Making House Calls
James’ parents both grew up in Oklahoma farming and ranching families. They met showing cattle in the Angus Association. After marrying, they settled on an acreage in Pond Creek, a town of 800 or so that sits more or less halfway between Enid and the Kansas border.
The land had been in James’ father’s family since before the Land Run. And though James, the oldest of three children, spent a good deal of time helping her dad farm and ranch, it was always clear that her future lay elsewhere. “I can’t remember not wanting to be a doctor,” she says.
As a child, her pastime of choice was something she called doll hospital. Instead of tea and imaginary crumpets, James would feed medicine (actually, crushed vitamins) to her Raggedy Ann and stuffed animals. She would also acquiesce to play store with her younger sister, but only, she says, if that store was a pharmacy and its “employees”—the James girls—“could pick up the medicine to deliver to the children of Nepal or the doll hospital.”
James suffered from asthma, a big problem if you live on a farm, so she visited the local pediatrician often. Even at a young age, she peppered her physician with questions. When she was 4, she remembers, “He said that if I wanted to become a nurse, he would hire me.” While presumably meant as a compliment, this did not sit well with the preschooler. “I told him that I would become a doctor and hire him.”
When James turned 12, an osteopath who regularly made house calls around the Pond Creek area invited her to tag along. “These were very sick people who couldn’t or wouldn’t see the doctor,” James recalls. They suffered from chronic health problems like diabetes, rheumatoid arthritis and congestive heart failure. Many never left their beds.
On and off through junior high and the early years of high school, James trailed the physician as he went from home to home. In between patients, she’d cross-examine him. Why is this diabetes patient improving while that one keeps getting sicker? How do you know which drug to give to which person? After four years, the osteopath offered her some frank career advice: You’re never going to be happy just practicing medicine, he said. You’re going to need to try research.
James took a job as a teller at a local bank so she’d have gas money to drive to an Enid hospital, where she volunteered as a candy striper. There, she spent time visiting with patients, some of whom were in the process of dying. From a young age, she’d played the organ at church—and also at many funerals. She’d already spent countless hours in the presence of the dead (“I didn’t recognize how strange that was until I got to medical school”), so she understood that “death is just part of the process; it’s just part of the circle of life.”
At the hospital, she enjoyed interacting with the staff. But what really cemented her decision to become a physician was the realization that she loved the patient contact, regardless of the outcome. “I felt comfortable with people who were sick or even dying.” Of course, she says, it was always more gratifying to see a baby born. “But for some who had suffered so much, death brought peace.”
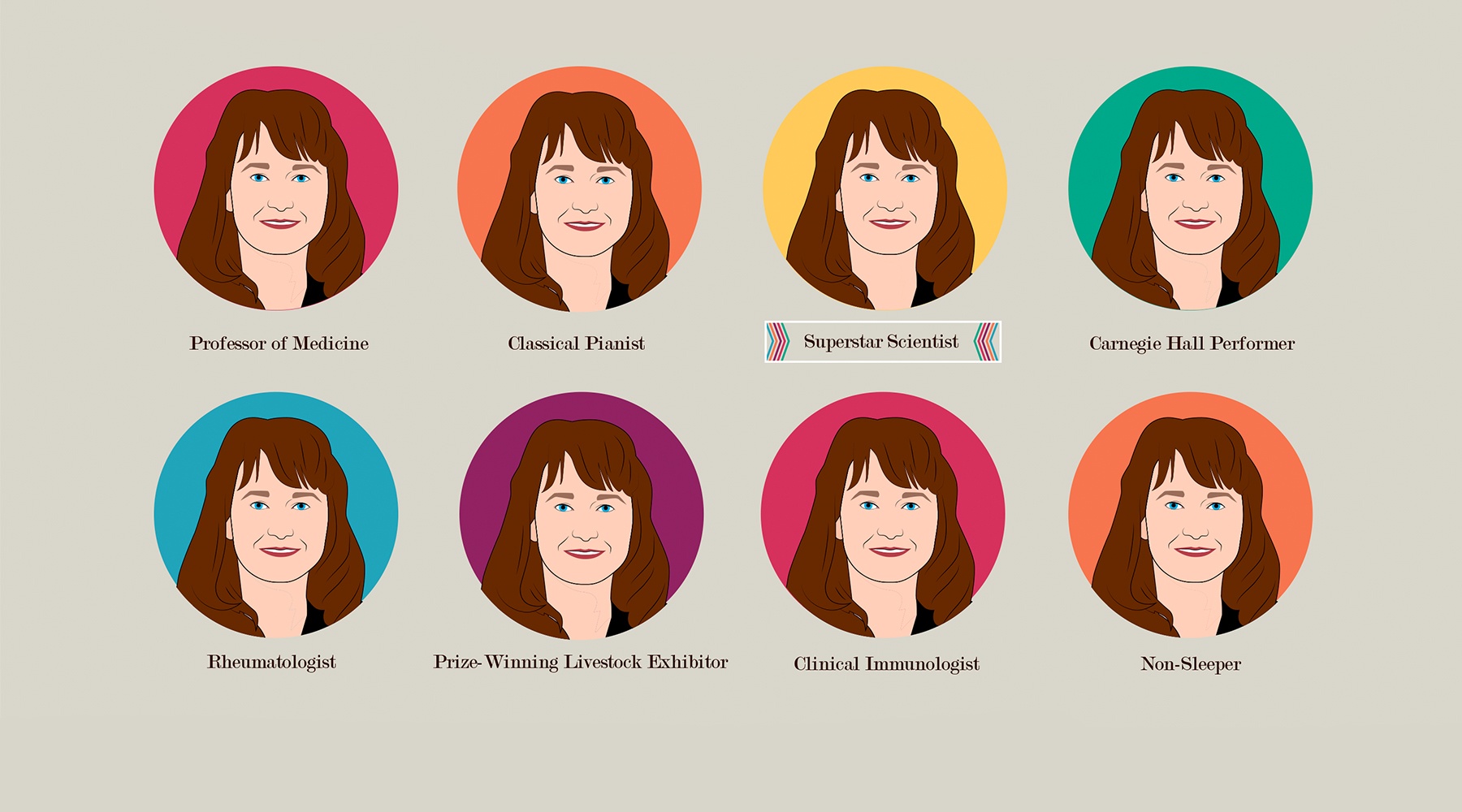
On the heels of an all-everything four years at Pond Creek High—cheerleader, a cappella singer, all-state pianist, prize-winning livestock exhibitor, valedictorian—James enrolled in the pre-med program at Oklahoma Baptist University. She came to OMRF the summer after her junior year as a Fleming Scholar. She’d told the selection committee she wanted to do research on asthma, a condition that not only afflicted her but also many members of her family. She was assigned to the laboratory of Dr. John Harley, a physician-researcher who was an allergist and rheumatologist.
At the time, scientists believed asthma might have a so-called autoimmune component. Autoimmune disorders are a family of more than 80 illnesses that include rheumatoid arthritis, type 1 diabetes and multiple sclerosis. In all of these conditions, the body’s immune system loses the ability to distinguish between its own healthy tissues and those of foreign invaders like bacteria and viruses. As a result, the immune system creates proteins that attack and destroy healthy tissue. These cellular assaults can cause inflammation, pain and damage to various parts of the body.
Harley assigned James a pair of projects to study different aspects of lupus, an autoimmune disease. Lupus primarily strikes women of childbearing age, and it most often affects the skin, joints and kidneys. Cases can range from mild to life-threatening. According to the Lupus Foundation of America, lupus is believed to affect 1.5 million Americans.
James thought her research on lupus would represent a brief scientific detour. “I figured I’d learn some autoimmunity, then apply it to asthma,” she says. But as she delved into the depths of the disease, investigating the molecular targets and the immune cells that mistakenly attack them, the work struck a chord with her. “I really liked the detective work. I enjoyed trying to figure out something that no one had figured out before.”
James returned to OBU for her senior year, but she kept working with Harley in OMRF’s labs. The University of Oklahoma Health Sciences Center launched an M.D./Ph.D. program, and on the strength of her undergraduate career and work in Harley’s lab, James was one of two students accepted into the inaugural class. This enabled her to simultaneously pursue a medical degree as well as a doctorate in microbiology and immunology.
In medical school, she initially had designs on becoming a pediatrician. But time and again, she found herself drawn to the rheumatology clinic. There, she saw people suffering from autoimmune diseases like lupus and rheumatoid arthritis, another condition that afflicted many in her family. “I was intrigued by the concept of autoimmunity, and I really liked the patients.” In particular, she saw an opportunity to improve the lives of those patients. “There were significant gaps in our knowledge of autoimmune diseases, and there were tremendous unmet treatment needs. Much of what we knew about these conditions—and the therapies we were using to treat them—were simply being borrowed from other fields.”
She did the research necessary to earn her Ph.D. in OMRF’s labs, publishing a variety of papers on lupus and securing grant funding while still a graduate student. Her doctoral thesis devised a way to identify abnormal immune responses in autoimmune diseases.
During her internal medicine and clinical training, she worked on OMRF’s scientific staff as a post-doctoral researcher. Working with Harley, she made major research strides. First, following up on her doctoral thesis, she was lead author of a research study on “epitope mapping,” the process of identifying the pieces of molecules that are targeted in autoimmune disease. Two years later, in a paper published in the Journal of Clinical Investigation, she showed lupus patients were more likely than the general population to have been exposed to a common childhood virus.
The research, all conducted while James continued to see patients, cast new light on autoimmune disorders, which, collectively, affect between 5 and 8 percent of the U.S. population. By the time OMRF promoted James to the role of principal investigator—meaning that she’d lead her own lab and independently map the course of her research projects—she’d also made a major finding about how immune responses in lupus patients changed over time. That discovery would earn her the Presidential Early Career Award for Scientists and Engineers from then-President Bill Clinton and lead to a seven-year grant from the National Institutes of Health.
James’ work to that point had studied how genetic and environmental factors work together to contribute to the development of lupus. In her short career, she’d already made key contributions to understanding how lupus progresses. Yet as she delved deeper into various aspects of the disease, she had a “What if?” moment.
“When I looked at the literature and all the studies being done on lupus, I realized the vast majority of the publications were based on data obtained after people had been diagnosed,” she says. Was there some way, she wondered, to predict who would ultimately develop lupus?
“With this kind of information, we could begin fighting disease before symptoms ever appear,” says James. Give physicians a diagnostic crystal ball, she thought, and they might be able to delay the onset of lupus. Perhaps they could even craft approaches that would lessen the brunt of the illness when it eventually reared its head.
The idea seemed like a reach—yet also a logical extension of the work James had already done. And if it proved successful, the payoff to patients could be huge. So she decided to give it a go.
A Crystal Ball for Lupus
Normally, the immune system relies on Y-shaped proteins known as antibodies to identify and neutralize foreign pathogens to the body. But in autoimmune diseases, certain rogue antibodies (known as “autoantibodies”) attack the body’s own cells.
Researchers had long known that these abnormal proteins could be found in people suffering from lupus and other autoimmune illnesses. Indeed, Dr. Morris Reichlin, James’ rheumatology mentor and colleague at OMRF, had done pioneering work in demonstrating how and why certain people’s bodies produce autoantibodies. But, James asked, when do they first show up? Is it possible they actually appear in the body before the first symptoms of disease?
The notion was striking. But there was one big hurdle: You can’t reverse time to test the blood of lupus patients before their first symptoms arose. James decided, she says, “to find a way to work backward.”
She knew that the U.S. military collected biological samples from enlisted personnel and kept those samples, along with the individuals’ medical records, for many years. If she and her research team could comb through tens of thousands of medical records and identify soldiers and sailors who eventually developed the disease, they could then request blood samples, taken before the onset of symptoms, and test them for autoantibodies.
Working with the then-chief of rheumatology at the Walter Reed Medical Center in Washington, D.C., James and the OMRF team—which also consisted of Harley and Dr. Hal Scofield—gained access to the U.S. Department of Defense serum repository. When they conducted their own testing on blood samples gathered from military personnel, the results were definitive: Of 130 servicemen and women who developed lupus, 88 percent had telltale autoantibodies before they showed clinical symptoms. Some of these markers appeared up to a decade before people became ill.
When James and her colleagues published the results of their research in the prestigious New England Journal of Medicine, “It made a very big splash in the lupus world,” says Dr. Jill Buyon, director of the division of rheumatology at New York University. “The idea that you could identify people who might later develop clinical autoimmunity was quite powerful.”
Indeed, the work held exciting potential for helping patients. Tests to detect these abnormal proteins could become a part of routine checkups for high-risk individuals, and a positive test could signal the need to take preventive action. The New York Times ran a story about the research, and Scientific American also featured it in a cover story entitled “New Predictors of Disease.”
But perhaps the highest compliment to the work came from her fellow autoimmune disease researchers. When scientists believe a paper has made important findings, they’ll cite it in their own publications. Think of prior research as a sort of building block upon which future findings are constructed.
A good paper may get cited a few dozen times. An influential one might hit the century mark. James’ New England Journal study has now been cited more than 1,000 times.
A New Focus
Since that watershed discovery, James has continued to build on the work. But as she peeled away the molecular layers, she found new subtleties. And those insights caused her to adjust the focus of her research.
“It turns out that just having certain antibodies doesn’t mean you’ll get sick,” she says. James and her research team found other events in the immune system, when coupled with the appearance of certain antibodies in the blood, signaled lupus would soon rear its head. Yet that knowledge was only useful to a point. “Even if you know it’s coming, that knowledge is only useful if you can do something to stop the disease. So what could we do to prevent lupus?”
Not surprisingly, James came up with an answer—or at least part of one—to her own question.
Using the biological samples and medical records she and her research team had gathered from the Department of Defense, James again decided she’d take a “backward” look at the 130 service members who ultimately developed lupus. This time, she centered her analysis on how quickly they went from showing early symptoms of the disease to full-blown lupus. Specifically, she was looking to see if there was any factor that might separate those who showed rapid disease onset from those whose illness progressed more slowly. And, eventually, she turned up an intriguing clue.
Some of the service members had been assigned to areas in which the mosquitoes carried malaria, a potentially deadly infectious disease. Twenty-six of them had received hydroxychloroquine, a medication used both to prevent and treat the mosquito-borne illness. When James examined their medical records and blood samples more closely, she realized they showed a longer time between the appearance of the first clinical symptom and the onset of full-blown lupus than those service members who had not been treated with the anti-malarial drug.
In other words, hydroxychloroquine appeared to delay the onset of lupus.
When James published her research in the journal Lupus, “It quite literally changed the way we practice medicine,” says Dr. Eliza Chakravarty, a rheumatologist who specializes in the treatment of pregnant women and was then a clinical faculty member at Stanford University. Based on the results of James’ study, when Chakravarty saw a patient who “had something that was not quite lupus, we’d immediately start treatment with hydroxychloroquine.” For the first time, says Chakravarty, physicians had a way to delay and possibly even halt the progression of lupus.
Subsequent scientific investigation has supported and expanded upon James’ initial findings on hydroxychloroquine. Rheumatologists now routinely prescribe it not only for patients displaying early symptoms but also as an ongoing therapy for those who’ve been diagnosed with lupus, with research showing the drug can reduce the frequency of disease flares and limit organ damage.
James is now helping to spearhead an “interventional” trial to find out whether hydroxychloroquine can prove similarly effective against rheumatoid arthritis, another autoimmune disease. Building on the approach pioneered in James’ New England Journal study, researchers have identified certain blood markers that predict—with 80 percent certainty—that a person will later develop RA. Together with physician-scientists at the University of Colorado, James and her team of OMRF rheumatologists are now enrolling patients who test positive for the biomarkers. They’ll give hydroxychloroquine to some, then compare their progress to untreated patients.
In addition, working with OMRF’s Drs. Melissa Munroe and Joel Guthridge, James has identified a number of biomarkers in the blood that predict when lupus patients are going to experience disease flares, which can range in severity from skin rashes to life-threatening fluid build-up around the heart or kidney failure. The pair is now working with a biotechnology company, Progentec Diagnostics, to transform the work into a test that will signal lupus flares even months in advance. “Even if patients aren’t feeling too bad, their immune systems are warning us a flare is coming,” says James. Armed with that knowledge, physicians can use a toolkit that consists of a variety of medications—including hydroxychloroquine—to prevent, or at least dampen the effects of, the coming disease storm.
It’s all, she says, part of an effort to deliver a course of therapy tailored to each lupus patient’s unique needs. “Unfortunately, there’s not a universal course of treatment for every lupus patient, and there are no perfect drugs.” Medications can help suppress symptoms, “but none of them actually stop the disease.” And many come with significant side effects. “So we want to pick the right drug for the right patient at the right time.”
Bringing relief to patients—hundreds of whom she still sees regularly as a rheumatologist in OMRF’s clinic—drives her research. And it animates the ultimate aim of all she does in the lab: to halt autoimmune diseases from ever taking hold. “Our goal,” she says, “is prevention.”
“The Best in the Entire Country”
Dr. Stephen Prescott is a cardiologist by training. For three decades, his research centered on vascular biology and the molecular genetics of disease. He’d never worked in the field of autoimmunity. But when he became OMRF’s president in 2006, he immediately saw James was, in his words, “a scientific superstar.”
Within a year of Prescott’s arrival, James took the reins of a major program grant at OMRF. The grant’s goal was to mentor junior scientists and enable them to establish successful independent research programs. And under James’ guidance, the junior investigators made impressive scientific strides. “Dr. James is driven, she’s organized, and she has the ability to motivate others,” says Prescott. In other words, “She has all the traits of a great leader.”
In 2008, Prescott named James the Lou C. Kerr Endowed Chair in Biomedical Research and head of a new department at OMRF, the Clinical Immunology Research Program. The program would study autoimmune diseases, but like James’ work, it would specialize in “translational” research, which is aimed at improving patient outcomes. Within a year, James successfully secured a $7 million grant from the National Institutes of Health to construct a new patient clinic and a massive biorepository, a state-of-the-art freezer facility where she and other OMRF physician-scientists could store biological samples donated by patient volunteers. When coupled with the carefully documented medical records they’d assemble in the clinic, these samples would—much like the serum repository at the Department of Defense that James had tapped for her earlier lupus studies—become an invaluable resource for OMRF researchers.
“Judith was years ahead of the curve in this area,” says Dr. P.J. Utz, a professor of medicine at Stanford University who studies autoimmune disease and also serves on OMRF’s external scientific advisory board. “When the scientific advisory board saw what she’d done—huge rooms filled with freezers and samples, plus great clinical data to go with those samples—we were just blown away.” With the significant investment of time, effort and funds required to build such a collection, few other institutions have done so. As a result, says Utz, “OMRF has cornered the market when it comes to clinical samples in autoimmune disease.”
Those samples and data have facilitated hundreds of research studies in lupus and other autoimmune disorders, including rheumatoid arthritis and multiple sclerosis, as well as less well-known conditions like Sjögren’s syndrome, scleroderma and sarcoidosis. They also proved a major asset in helping James to secure another major program grant for OMRF from the National Institutes of Health—an Autoimmunity Center of Excellence award. That designation, one of fewer than a dozen given nationwide, placed OMRF in elite company. Along with Stanford, Yale, Duke and a handful of other institutions, OMRF shared in an award of more than $50 million to fund laboratory and clinical research aimed at developing treatments for lupus, rheumatoid arthritis and other autoimmune disorders.
A year after the Autoimmunity Center of Excellence award, Prescott made the decision to merge James’ department with OMRF’s Arthritis and Immunology department. With more than 150 staff members, the newly combined Arthritis and Clinical Immunology Research Program would focus on both laboratory and translational studies of rheumatologic and autoimmune diseases. And James would lead it.
In the half-dozen years since, the clinical and laboratory researchers in the program have thrived. They’ve published more than 400 new research studies in peer-reviewed scientific journals. They’ve opened the Multiple Sclerosis Center of Excellence, which now treats 2,500 MS patients, oversees clinical trials of more than a dozen investigational new drugs, and enrolls patient volunteers in a wide range of research studies. In 2014, OMRF was again designated as an Autoimmunity Center of Excellence. And scientists in this group secured a series of new grants that have helped the program grow, by the addition of both new laboratory projects and researchers.
One of those who made the decision to relocate to OMRF was Stanford’s Chakravarty. “I wasn’t looking to leave Palo Alto, but I met Judith at a small lupus conference,” she says. “I’d always followed her work, so when she asked me to get together, I said, ‘Sure.’” James, who Chakravarty describes as one of her ‘heroes,’ surprised Chakravarty over lunch by inquiring if she’d be interested in moving from California to Oklahoma City.
To be, in her words, “polite,” Chakravarty agreed to visit OMRF, but she had no real intention of moving—until she arrived at the foundation. “After the first two interviews, I was sold.” Five years later, she couldn’t be happier about her decision to join OMRF. “Under Judith’s mentorship, I have been able to transform my career from clinical to translational research. And I got my first National Institutes of Health grant”—a major milestone in the career of any researcher—“largely because of her. She’s amazing at reviewing grants before you submit them. She knows the field so well, and she gives incredible constructive criticism.”
Indeed, this well-honed skill for “grantsmanship” has been one of the cornerstones of James’ success as a leader. In particular, she’s continued to lead efforts to secure new collaborative federal grants that have helped OMRF researchers form partnerships with scientists and clinicians at other institutions. Those initiatives have included a Native American Research Centers for Health grant, where she and OMRF physician-scientists teamed with a network of Oklahoma tribes to improve outcomes for tribal members suffering from autoimmune disease. She also led the effort to create the Oklahoma Shared Clinical and Translational Resource, a partnership with the University of Oklahoma Health Sciences Center (where she holds appointments as a professor of medicine and associate vice provost) and more than a dozen other state and tribal organizations. Funded by a $20 million National Institutes of Health grant, the initiative aims to improve clinical and translational medicine in the state, with a focus on underserved rural populations.
Finally, teaming with Stanford’s Utz and physician-scientists at the University of Colorado, she helped secure one of the first of the so-called AMP grants. AMP (which stands for Accelerating Medicines Partnership) couples academic and nonprofit researchers with biopharmaceutical companies. Designed to speed the development and delivery of new diagnostics and therapies to the clinic, James is part of a team that’s working on autoimmune disorders, one of three disease targets—along with Alzheimer’s and diabetes—of the program, a joint initiative of the National Institutes of Health and the Food and Drug Administration.
If all of this sounds overwhelming, it is.
“Judith is the hardest worker I know,” says New York University’s Buyon. “I can’t count the number of times I’ve gotten long, exquisitely detailed emails from her at 1 in the morning. She’s indefatigable.”
Still, says OMRF’s Chakravarty, “For somebody who packs so much into her day, you always feel like she has time to mentor you. I don’t know how she does it.”
In the world of autoimmunity research, says Utz of Stanford, “Judith is viewed as an absolute superstar. But what separates her from everybody else is her selflessness.” An avid Golden State Warriors fan, Utz likens James’ scientific work to the on-court performance of a certain NBA player. “She was the Kevin Durant of autoimmunity research. But now she’s evolved from being a fabulous player to being a great coach. I can honestly say that among rheumatology division chiefs, she’s the best in the entire country.”
Family Matters
Every few months or so, James finds her way back to the family farm in Pond Creek. She’ll also occasionally make her way down to Verden, where she sits with her grandmother and other members of her family in the front two rows of the local church. “I grew up on a farm outside of a small town, so these are the places where I’m comfortable.”
James still likes to play the piano, but she no longer plays in front of people. She did have the chance a few years ago to fulfill a lifelong dream of singing at Carnegie Hall, where she performed as part of a choir. But mostly, she and her husband of 22 years, Glen Wood, who teaches history in Edmond Public Schools, devote any spare time to their daughter, Becca.
A senior at Piedmont High, Becca’s high school career bears a striking resemblance to that of her mother: She’s an honors student, a singer, and an all-state swimmer. Not surprisingly, it seems that Becca also hears the call of medicine and research. “She says she wants to complete an M.D./Ph.D. in infectious disease and run a clinic for difficult-to-diagnose diseases,” says James.
Like so many parents, James feels a bit conflicted about her daughter’s potential career choice. “It makes me excited, but at the same time it makes me nervous. Because I wish she would find an easier path.” She thinks for a second. “But if this is what she’s called to do, she needs to do it, whether it’s hard or not.”
With that, James must go. It’s after 5 p.m., but her day is far from over. She’s finished with meetings, managing lab and departmental operations, and seeing patients, but she still has a conference call with a collaborator, a grant to write and, of course, a 17-year-old to help raise.
Did she ever imagine this is where milking a tarantula would lead?
James smiles. Following the spider project, she was offered the chance, she says, “to spend the summer in Honduras as a great tarantula hunter.” Perhaps that might have paved the way for her to become the arachnid world’s Indiana Jones. Instead, she chose to come to OMRF.
Since then, she’s mentored almost 100 students and trainees in her lab. She’s treated thousands of patients suffering from lupus and other autoimmune diseases. In some cases, she’s now taking care of the second and third generation of patients from the same families.
It’s a gift, she knows, to be able to bring relief to people in pain. To nurture young people’s careers. To cast light on scientific mysteries no one before had solved.
No, this isn’t precisely the road she had imagined. But it’s been a rewarding journey. And it’s one, she hopes, that still has many intriguing destinations ahead.