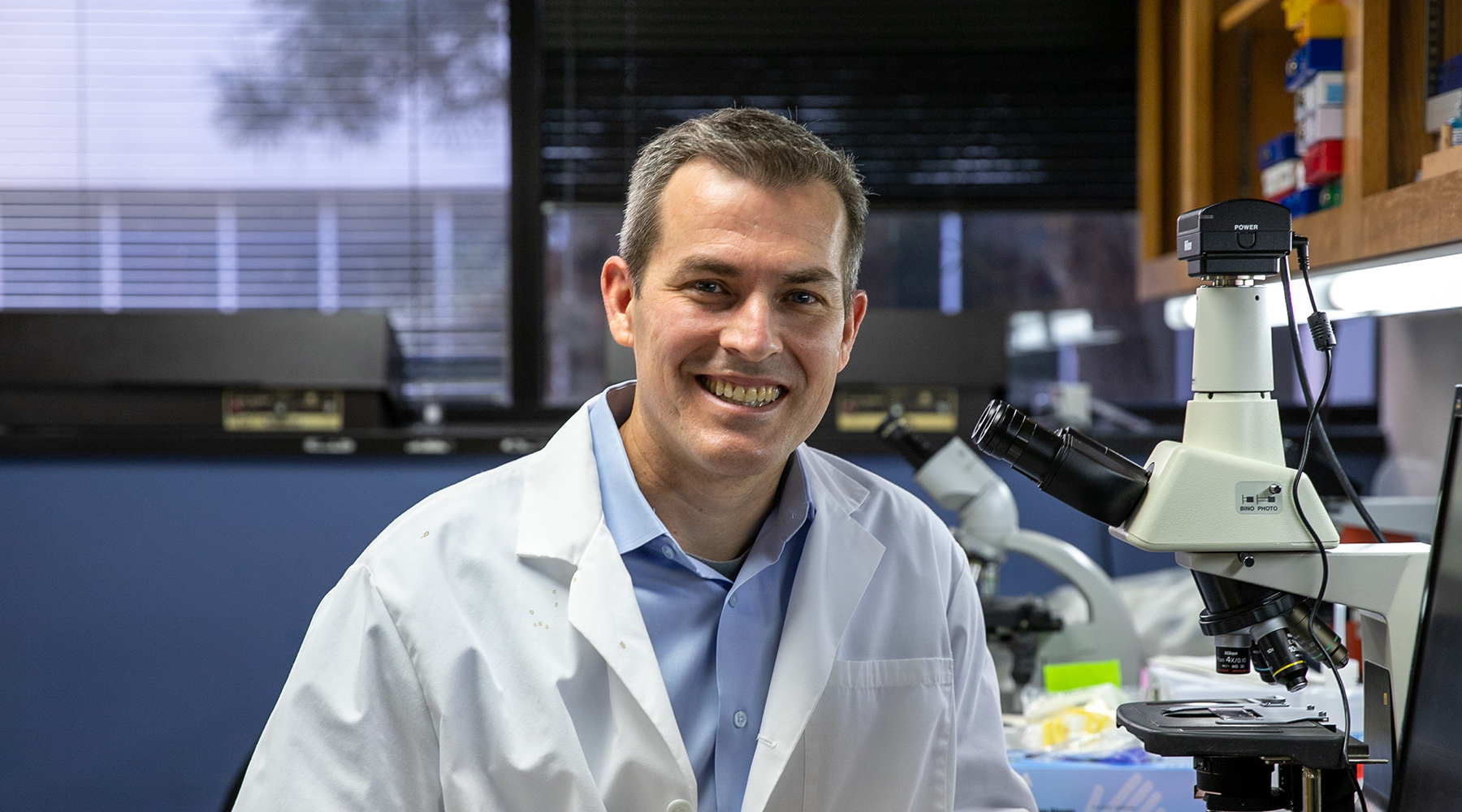
Timothy M. Griffin, Ph.D.
Associate Professor
Aging & Metabolism Research Program
Research Biologist, Adjunct Associate Professor, Department of Physiology and Department of Biochemistry and Molecular Biology, University of Oklahoma Health Sciences Center
Member, Geroscience and Healthy Brain Aging and Oklahoma Center for Neuroscience, University of Oklahoma Health Sciences Center
My 101
When we imagine retirement, we often picture ourselves traveling to new lands and getting back in touch with nature through gardening or taking hikes. We take for granted that our bodies will carry us forward into these hard-earned dreams. However, for over 32 million Americans, these dreams may be put on hold due to joint pain and stiffness caused by osteoarthritis. Osteoarthritis is the most common form of arthritis, and it’s the leading cause of disability in the U.S. My lab is studying how this disease begins and how we can treat people already suffering from it.
The chances of developing osteoarthritis increase as we age, put on weight, or injure our joints. Although conventional wisdom holds that increased pressure on joints from carrying excess weight causes osteoarthritis, this is far from a complete answer. Recent discoveries suggest that fat itself is a critical mediator of the disease. Fat is not just storing excess energy from food. Rather, fat acts like an organ by releasing molecules that affect how the body functions. When the body has too much fat, it can release molecules that activate immune cells and cause inflammation.
My lab is studying how obesity alters the metabolic machinery of tissues and cells within the joint. We believe that excess fat causes metabolic changes that promote joint inflammation, tissue damage, and ultimately joint pain. Luckily, these negative effects of excess fat can be reversed through exercise, even without weight loss. Many studies show that staying active is the best way to reduce osteoarthritis pain. Therefore, we're also studying how exercise breaks the cycle of metabolic inflammation and pain to develop new treatment options for people to live more active lives free from limitations. By focusing on the metabolic basis of osteoarthritis, we expect to open up new treatment strategies by painting a more complete picture of this costly disease.
Research
Osteoarthritis is a disease characterized by cartilage destruction and abnormal bone growth resulting in joint pain and severe disability. It is the primary cause of disability in the United States, and it contributes significantly to reductions in health that occur with aging. Although osteoarthritis is often considered an inevitable consequence of aging, numerous genetic and environment risk factors have been identified that mediate its occurrence and severity. One of the most significant and modifiable risk factors is obesity.
Our laboratory uses integrative and interdisciplinary approaches to study how obesity dysregulates biomechanical, inflammatory, and metabolic processes that are associated with the development of osteoarthritis. We are seeking to determine how dietary fats, adipokines (e.g., leptin), and cyclic joint loading regulate articular cartilage homeostasis via effects on chondrocyte mitochondrial function and free radical biology. We are particularly interested in the role of sirtuins (e.g., Sirt3) as regulators of cellular metabolism and oxidative stress responses that help maintain chondrocyte function during aging, obesity, and injury. In addition, we are investigating how intra-articular adipose tissue modulates joint inflammation by altering the metabolic environment of the joint.
We are also interested in understanding how physical activity interacts with obesity-related phenotypes to regulate these processes in healthy and diseased tissue. Therefore, we use a variety of models spanning multiple levels of organization (e.g., cell, tissue, and animal) to study the effect of voluntary exercise (in vivo) and controlled biomechanical loading regimes (in vitro) on inflammatory, metabolic, and anti-oxidant processes in cartilage.
By studying the interaction of diet and physical activity (i.e., two modifiable risk factors for obesity) during aging, we hope to reveal novel pathways that regulate cartilage matrix homeostasis. Furthermore, by examining behavioral changes in our animal models that are associated with motor function and pain, we emphasize clinically relevant outcome measures so that we can better translate our finding to patients. These studies provide a basis for examining how therapeutic interventions that target inflammatory, metabolic, or oxidative processes affect joint-specific pathophysiology and functional outcomes.
Brief CV
Education
B.A., Harvard University, Cambridge, MA, 1996
Ph.D., University of California, Berkeley, CA, 2002
Postdoc, Duke University Medical Center, Durham, NC, 2002–2007
Honors and Awards
New Investigator Award, American Physiological Society, 2003
NIH Ruth L. Kirschstein National Research Service Award, NIAMS, 2004
Hulda Irene Duggan Arthritis Investigator Award, Arthritis Foundation, 2007
Young Investigator Award, Osteoarthritis Research Society International World Congress on Osteoarthritis, 2007
Outstanding Postdoc Award, Duke University, 2007
Melba M. O’Connell Memorial Fellow, Arthritis National Research Foundation, 2010
Top 10 Arthritis Advances, Arthritis Foundation, 2010
Fred Jones Award for Scientific Achievement, Oklahoma Medical Research Foundation, 2016
Arthritis Foundation Medical Honoree, OKC Arthritis Walk, 2018
Health Care Hero, The Journal Record, 2020
Merrick Award for Outstanding Medical Research, 2020
Professional Activities
Invited Participant, NIH NIAMS Roundtable on OA and Inflammation, 2013
Advisory Editor, Arthritis & Rheumatology, 2013-2016
Co-chair, Cartilage, Synovium & Osteoarthritis Topic Committee, Orthopaedic Research Society, 2014-2016
Member, NIH NIAMS Biospecimen Review and Allocation Committee for the Osteoarthritis Initiative, 2015-present
Section Leader (OA Laboratory Grants), Arthritis Foundation's Delivering on Discovery Peer Review, 2015
Editorial Board Member, Osteoarthritis and Cartilage, 2016-2019
Ad hoc reviewer, SBSR Study Section, NIH, 2017-present
Associate Editor, Osteoarthritis and Cartilage, 2019-present
Memberships
American Physiological Society
Orthopaedic Research Society
Osteoarthritis Research Society International
Joined OMRF scientific staff in 2008
Publications
Recent Publications
Komaravolu RK, Mehta-D'souza P, Conner T, Allen M, Lumry J, Batushansky A, Pezant NP, Montgomery CG, Griffin TM. Sex-specific effects of injury and beta-adrenergic activation on metabolic and inflammatory mediators in a murine model of post-traumatic osteoarthritis. Osteoarthritis Cartilage, 2024 March, PMID: 38527663
South SM, Marlin MC, Mehta-D'souza P, Stephens T, Conner T, Burt KG, Guthridge JM, Scanzello CR, Griffin TM. Imaging mass cytometry reveals tissue-specific cellular immune phenotypes in the mouse knee following ACL injury. Osteoarthr Cartil Open 5:100416, 2023 November, PMID: 38107076, PMCID: PMC10724482
Hahn AK, Rawle RA, Bothner B, Prado Lopes EB, Griffin TM, June RK. In vivo mechanotransduction: Effect of acute exercise on the metabolomic profiles of mouse synovial fluid. Osteoarthr Cartil Open 4:100228, 2021 December, PMID: 36474473, PMCID: PMC9718234
Selected Publications
Griffin TM, Batushansky A, Hudson J, Lopes EBP. (2020) Correlation Network Analysis Reveals Distinct Systemic Links To Osteoarthritis in Mice: Effects of Long-Term High Fat Diet and Exercise. J Health and Sport Science (Special Issue on Exercise, Metabolism, Obesity, and Musculoskeletal Health). 9(2):119-131. doi.org/10.1016/j.jshs.2019.05.008.
Griffin TM, Lories RJ. (2020) Cracking the code on the innate immune program in OA. Osteoarthritis and Cartilage. 28(5):529-531. PMID: 32278072
Griffin TM, Friedman JE. (2020) How can parental obesity promote OA across generations? Nature Rev Rheumatology. 16(3):129-130. PMID: 31949286
Andriacchi TP, Griffin TM, Loeser Jr RF, Chu CR, Roos EM, Hawker GA, Erhart-Hledik JC, Fischer AG. (2020) Bridging Disciplines as a pathway to Finding New Solutions for Osteoarthritis a collaborative program presented at the 2019 Orthopaedic Research Society and the Osteoarthritis Research Society International. Osteoarthritis and Cartilage Open. March;2(1):100026. doi.org/10.1016/j.ocarto.2020.100026
Zhu S, Makosa D, Miller BF, Griffin TM. (2020) Glutathione as a mediator of cartilage oxidative stress resistance and resilience during aging and osteoarthritis. Connective Tissue Research. Jan;61(1):34-47. doi: 10.1080/03008207.2019.1665035. Epub 2019 Sep 15. PMID: 31522568, PMCID: PMC6884680
Batushansky A, Lopes EBP, Zhu S, Humphries KM, Griffin TM. (2019) GC-MS Method for Metabolic Profiling of Mouse Femoral Head Articular Cartilage Reveals Distinct Effects of Tissue Culture and Development. Osteoarthritis and Cartilage. 27(9);1361-1371. PMID: 31136803, PMCID: PMC6702098
Contact
Aging & Metabolism Research Program, MS 46
Oklahoma Medical Research Foundation
825 N.E. 13th Street
Oklahoma City, OK 73104
Phone: (405) 271-7579
Fax: (405) 271-1437
E-mail: Tim-Griffin@omrf.org
For media inquiries, please contact OMRF’s Office of Public Affairs at news@omrf.org.
News from the Griffin lab
A new wave of researchers has joined the Oklahoma Medical Research Foundation’s scientific staff as part of the foundation’s expansion. OMRF has added seven new scientists to its staff. In addition, two research assistants have been promoted to faculty-level positions. The new researchers have come to OMRF from a variety of institutions across the U.S. […]