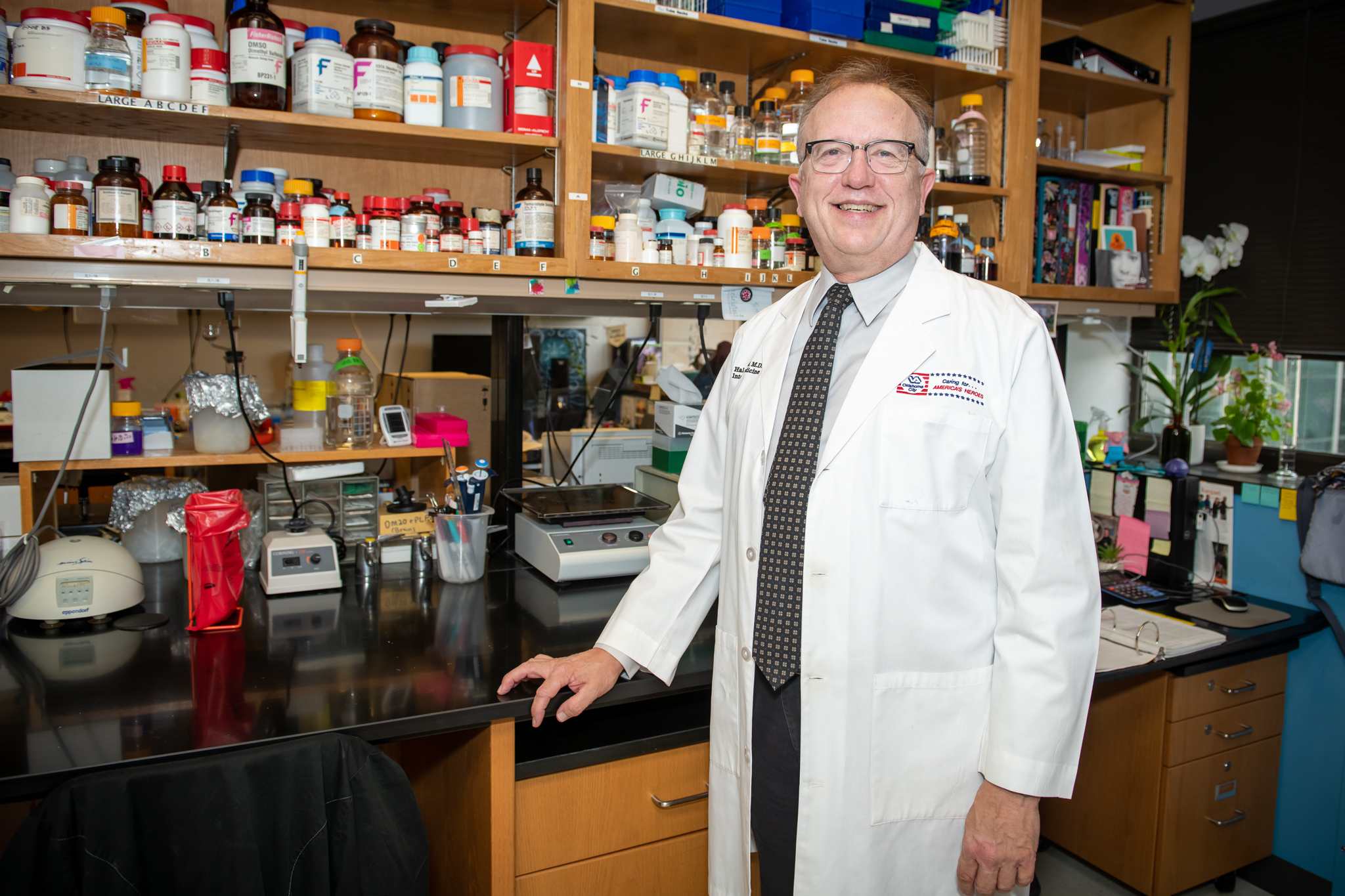
Robert H. “Hal” Scofield, M.D.
Professor
Arthritis & Clinical Immunology Research Program
Adjunct Associate Professor, Department of Pathology and Department of Medicine, University of Oklahoma Health Sciences Center
My 101
Normally the immune system protects the body from harmful bacteria and viral infections. But in autoimmune diseases, the immune system turns against the body, causing weakness, pain, and organ dysfunction, and sometimes leads to premature death.
In my laboratory, we’re working toward a better understanding autoimmune disease. In general autoimmune disease effects women much more commonly than men. For instance, 90% of lupus and Sjögren’s syndrome patients are women. That is, men are 10 times less likely to have these diseases than women. The sex chromosome are X and Y – women have two X chromosomes, while men have an X and a Y. However, we have found that men with an extra X chromosome, which occur in about 1 in 500 male births, have some autoimmune diseases at the same rate as women. In addition, women with three X chromosomes also have increased risk of autoimmune disease. We are now exploring the molecular and genetic basis by which an extra X chromosomes gives risk of autoimmunity.
We’re also looking at the genetics and immunology of both systemic lupus erythematosus, more often called just lupus, and the related Sjögren’s syndrome. We’re interested in how these diseases differently affect ethnic groups such as Native and African Americans. African Americans are more likely to have lupus and to have more severe cases of the disease, while Native Americans are more likely to have Sjögren’s syndrome. We are studying how antibodies, usually made to fight against viruses and bacteria, may cause these autoimmune diseases.
In conjunction with the US Department of Veterans Affairs, we have recently begun a project to examine autoimmune disease among those with post-traumatic stress disorder. Those with PTSD have 2 or 3 times more lupus, rheumatoid arthritis, multiple sclerosis and autoimmune thyroid disease then those with PTSD. We’re studying how the immune system is abnormal in PTSD patients.
Research
My laboratory studies the immunology, genetics and clinical expression of the autoimmune diseases systemic lupus erythematosus and Sjögren’s syndrome. Like most autoimmune disease, lupus and Sjögren’s predominately affect women, with ~90% of patients being female. For years those interested in lupus and Sjögren’s asked why women have these diseases. A few years ago we reversed the question and asked why some men get lupus or Sjögren’s. In order to facilitate answering such a question, we collected the largest cohort of men with lupus ever assembled as well as large group of men with Sjögren’s. We found that among these men, Klinefelter’s syndrome (47,XXY, 1 in 500 live male births) was over-represented about 15-fold. Klinefelter men have an extra X chromosome; that is, are 47,XXY while normal men are 46,XY. In addition, we found that women with an extra X chromosome (47,XXX, 1 in 1000 live female births) were found more than expected by chance alone among women with these diseases. In cells with more than one X chromosome, all but one is inactivated, but this in activation is not complete in that some X chromosome genes escape inactivation. We are now studying the molecular and immunological basis of the X chromosome dose effect. These studies concentrate on genes on the X chromosome that escape inactivation and whose protein products are critical to the immune system, especially interferon production. Understanding the female bias of autoimmune disease at a fundamental level will be a critical step forward.
Antibodies are produce by the immune system against foreign invaders such as bacteria and virus. In autoimmune disease, antibodies are produced against self. We are studying how such antibodies are involved in the pathogenesis of Sjögren’s syndrome. We produced recombinant, human monoclonal antibodies from B lymphocytes purified from the salivary glands of Sjögren’s patients. In this way we can study the disease causing potential of these auto-antibodies. Our results indicate that autoantibodies are produced in the salivary glands of Sjögren’s patients. These antibodies can impair saliva production perhaps by binding muscarinic receptors. In addition, unusual glycosylation of antibodies can lead to autoimmunity.
Post-traumatic stress disorder is common in the general population and is associated with an increased risk of autoimmune diseases, including lupus, rheumatoid arthritis, multiple sclerosis and thyroid disease. In a recently started project, we are studying autoantibodies as well as B lymphocytes hyperactivity in PTSD. We hypothesize that there are immune abnormalities that predispose to both PTSD and autoimmune disease. Alternatively, PSTD might induce immune alterations that then give rise to autoimmunity. Our work should be able to distinguish these two possibilities.
Infection with Epstein-Barr virus (EBV, the causative agent of mononucleosis, may be important in the genesis of lupus and Sjögren’s syndrome. We are determining whether the Epstein Barr nuclear antigen 2 (EBNA2), a genetic transcription factor, binds to genes that increase the risk of Sjögren’s syndrome. In addition, we will determine whether EBNA2 is expression salivary gland from Sjögren’s patients. These studies should develop a pathophysiological basis by which EBV infection may be permissive for development of autoimmune disease.
Brief CV
Education
B.A., Texas A&M University, 1980
M.D., University of Texas Southwestern Medical School, Dallas, 1984
M.A., Johns Hopkins University, Exp. 2023
Honors and Awards
Distinguished Student, Texas A&M University
Stewart Wolf Award as Outstanding Medicine Resident, 1987
W.W. Rucks Fellowship, 1988-1989
Presbyterian Health Foundation Fellowship, 1989-1991
Visiting Professor’s Award, 1989
Outstanding Paper, OUHSC Housestaff Scientific Session, 1989
Best Paper in Internal Medicine, OUHSC Housestaff, Scientific Session, 1990
Lloyd Rader Scholarship, Outstanding Postgraduate Trainee, OUHSC, 1990
Physician Scientist Award, NIH, Institute of Musculoskeletal and Skin Diseases, 1992-1997
The Merrick Award for Outstanding Research, OMRF, 1992
Internal Medicine Faculty Teaching Award, Department of Medicine, OUHSC, 1995
OUHSC Provost Award for research by an Assistant Professor, 1996
Henry Christian Award, American Federation of Medical Research national meeting, 1994
Fellow, American College of Physicians, 1998
James A. Shannon Director’s Award, NIAMS and the Office for Research on Women’s Diseases, 2001
OUHSC Provost Award for research by a senior faculty member, 2002
Oklahoma Health Research Committee, appointed by Governor Brad Henry, 2003-2018
Ethel Baxter Award for Outstanding Sjogren’s Syndrome Abstract, American College of Rheumatology National Meeting, 2004
Federation of Clinical Immunology Societies national meeting Travel Award, 2006
University of Oklahoma Board of Regents Award for Superior Creative Activity, 2014
Cecil Martin Distinguished Lecturer, Southern Illinois College of Medicine, 2015
Keynote Speaker, Six Southern Chinese Provinces Rheumatology Meeting, Changsha, China, 2015
Keynote Speaker, Korean Rheumatology Society, Seoul, Korea, 2016
Lewisville High School Hall of Fame inductee, 2016
James F Hammarsten Physician of Excellence Award, Oklahoma City Department of Veterans Affairs Health Care Center, 2018
Fellow, Southern Society of Clinical Investigation, 2019
Other Activities
Serves as Associate Chief of Staff for Research at the Oklahoma City Department of Veterans Affairs Medical Center; Chair, Pharmacy & Therapeutics Committee, OKC VAMC; Member, Clinical Competency Committee, internal medicine residency program, OUHSC Department of Medicine; Member, International Sjögren's Syndrome Criteria Working Group; Executive Committee and Co-Chair, Pulmonary Sub-committee Sjögren’s Syndrome Foundation/American College of Rheumatology Working Group for Sjögren’s Treatment Guidelines; Member, Publications Committee, American College of Rheumatology; volunteer physician, Good Shepard Clinic; Member, Concert and Jazz Band, New Horizons International Music Association, University of Oklahoma.
Memberships
American College of Physicians
American College of Rheumatology
American Federation of Clinical Research
The Endocrine Society
American Association for the Advancement of Science
American Diabetes Association
Oklahoma Rheumatism Association
The Society of General Internal Medicine
The New York Academy of Sciences
American Association of Immunologists
Joined OMRF scientific staff in 1991
Publications
Recent Publications
Kurien BT, Scofield RH. Current Trends in Validating Antibody Specificities for ELISpot by Western Blotting. Methods Mol Biol 2768:15-27, 2024 January, PMID: 38502385
George CT, Kurien BT, Scofield RH. The Potential Utility of Salivary and Tear Proteomics to Discriminate Sjögren's Disease from Non-Sjögren's Sicca. Int J Mol Sci 24, 2023 December, PMID: 38139325, PMCID: PMC10744321
Igoe A, Merjanah S, Harley ITW, Clark DH, Sun C, Kaufman KM, Harley JB, Kaelber DC, Scofield RH. Association between systemic lupus erythematosus and myasthenia gravis: A population-based National Study. Clin Immunol:109810, 2023 November, PMID: 37949200
Selected Publications
Harris VM, Koelsch KA, Kurien BT, Harley ITW, Wren JD, Harley JB, Scofield RH. Characterization of cxorf21 Provides Molecular Insight Into Female-Bias Immune Response in SLE Pathogenesis. Front Immunol. 2019 Oct 21;10:2160. PMID: 31695690 PMCID: PMC6816314
Harris VM, Harley ITW, Kurien BT, Koelsch KA, Scofield RH. Lysosomal pH Is Regulated in a Sex Dependent Manner in Immune Cells Expressing CXorf21. Front Immunol. 2019 Apr 2;10:578. PMID: 31001245 PMCID: PMC6454867
Scofield RH, Sharma R, Pezant N, Kelly JA, Radfar L, Lewis DM, Kaufman CE, Cioli S, Harris J, Grundahl K, Rhodus NL, Wallace DJ, Weisman MH, Venuturupalli S, Brennan MT, Koelsch KA, Lessard CJ, Montgomery CG, Sivils KL, Rasmussen A. American Indians Have a Higher Risk of Sjögren's Syndrome and More Disease Activity Than European Americans and African Americans. Arthritis Care Res (Hoboken). 2020 Aug;72(8):1049-105 PMID: 31199565, PMCID: PMC6911033
Basu A, Izuora K, Betts NM, Kinney JW, Salazar AM, Ebersole JL, Scofield RH. Dietary Strawberries Improve Cardiometabolic Risks in Adults with Obesity and Elevated Serum LDL Cholesterol in a Randomized Controlled Crossover Trial. Nutrients. 2021 Apr 23;13(5):1421. doi: 10.3390/nu13051421. PMID: 33922576, PMCID: PMC8145532
Park EH, Ha YJ, Kang EH, Song YW, Scofield RH, Lee YJ. Baseline disease activity influences subsequent achievement of patient acceptable symptom state in Sjögren's syndrome. Rheumatology (Oxford). 2021 Jun 18;60(6):2714-2724. PMID: 33188390
Lee AS, Scofield RH, Hammitt KM, Gupta N, Thomas DE, Moua T, Ussavarungsi K, St Clair EW, Meehan R, Dunleavy K, Makara M, Carsons SE, Carteron NL; Consensus Expert Panel (CEP) Members. Consensus Guidelines for Evaluation and Management of Pulmonary Disease in Sjögren's. Chest. 2021 Feb;159(2):683-698. PMID: 33075377
Contact
Arthritis & Clinical Immunology Research Program, MS 38
Oklahoma Medical Research Foundation
825 N.E. 13th Street
Oklahoma City, OK 73104
Phone: (405) 271-7144
Fax: (405) 271-7063
E-mail: Hal-Scofield@omrf.org
For media inquiries, please contact OMRF’s Office of Public Affairs at news@omrf.org.
Lab Staff
Biji Kurien, Ph.D.
Staff Scientist
Joshua Cavett
Research Technician III
DeVavrat Dave
Research Technician
Dashari Miller
OMRF Langston University Biomedical Research Laboratory Technician
Christina Bruxvoort
Graduate Student
Martha Tsaliki
Graduate Student
Rebecca Wood
Graduate Student
Valerie Lewis, Ph.D.
Affiliate
Stephanie Lawrence
Affiliate
Nyeisha Caldwell
Administrative Assistant IV
News from the Scofield lab

If he’s not conducting research or caring for patients, Dr. Hal Scofield has a staggering array of passions that keep him busy. And the list is always growing. By Adam Cohen | Illustrations by Jeffrey Smith When his late mother was in the early phases of dementia, Dr. Hal Scofield and his younger daughter, Amanda, headed […]
The new millennium began with a bang at OMRF, as Dr. Jordan Tang, above, and his research team identified and cloned the enzyme believed to cause Alzheimer’s disease. Soon after, the OMRF scientists designed an inhibitor that stopped the enzyme in its tracks. The discoveries led to the development of an experimental drug acquired by […]
You may never have heard of Sjögren’s syndrome, but you may very well know someone suffering from the illness. Sjögren’s (pronounced SHOW-grins) is a chronic autoimmune disease in which the body’s white blood cells attack the moisture-producing glands. The hallmark symptoms are dry eyes and dry mouth, but Sjögren’s may also cause dysfunction of other […]
In a study published tomorrow in The New England Journal of Medicine, scientists report that in patients suffering from systemic lupus erythematosus (commonly known as lupus), autoantibodies – proteins that the body mistakenly unleashes against its own tissue – are typically present years before patients are diagnosed with the disease. This research by scientists at […]
Patients who suffer with this autoimmune disease, as well as physicians who treat it, will gather in Oklahoma City Saturday, October 31 for the Ninth Annual National Conference for Sjogren’s Syndrome (NSSA). Chairman of the symposium is Morris Reichlin, M.D., Head of the Arthritis and Immunology Research Program at the Oklahoma Medical Research Foundation and […]