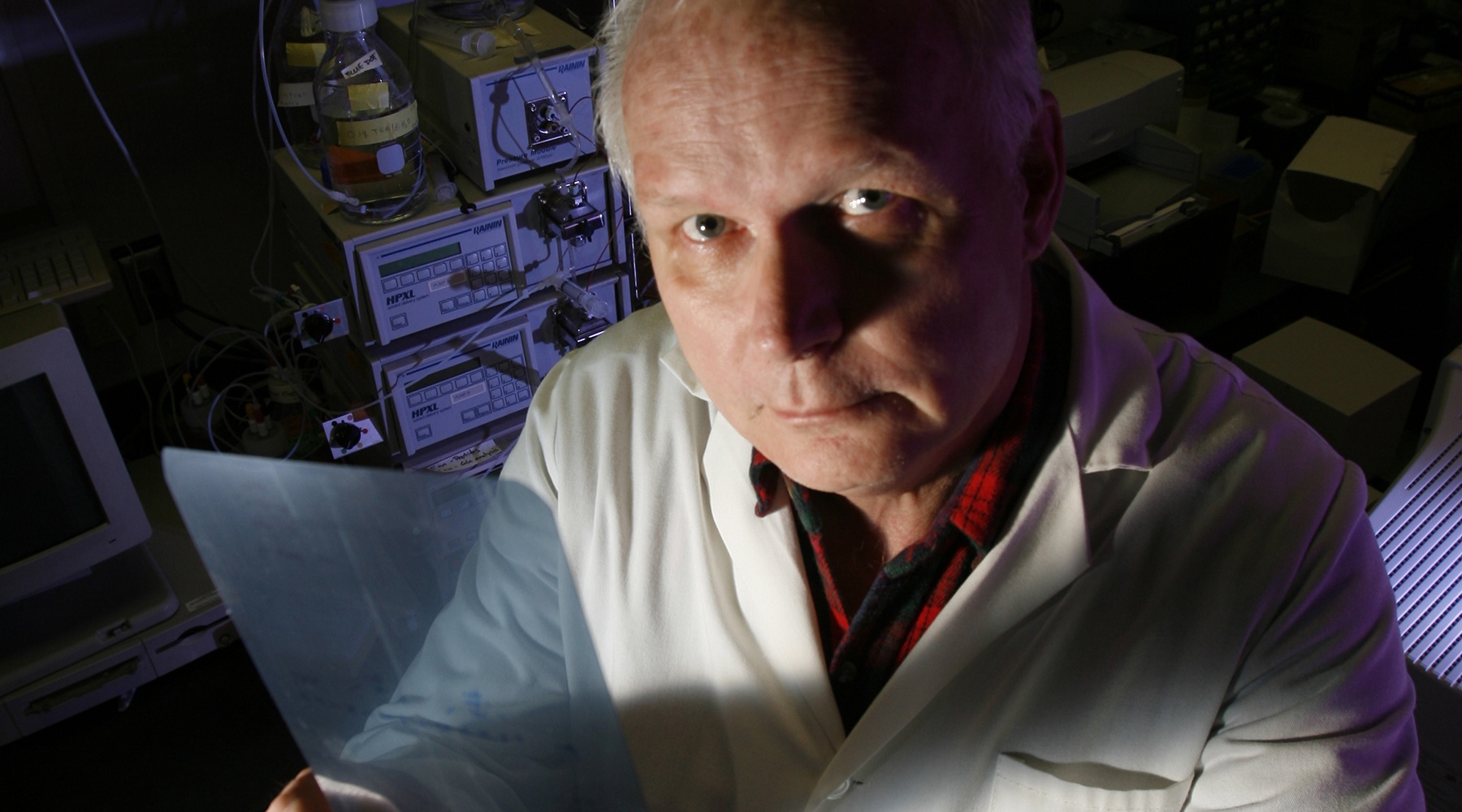
Charles T. Esmon, Ph.D.
Distinguished Career Scientist
Member, National Academy of Sciences
Adjunct Professor, Departments of Biochemistry & Molecular Biology and Pathology, University of Oklahoma Health Sciences Center
My 101
In my lab, we studied the mechanisms that control the process of blood clotting and the links between the controls of blood clotting and inflammation.
Blood clots are the cause of many serious human diseases, including heart attacks, strokes, pulmonary emboli, and venous thrombosis (phlebitis). They contribute to the mortality and morbidity of septic shock, acute trauma injury, and some of the complications of diabetes.
To understand why abnormal clots occur, we examined the mechanisms by which the normal blood-clotting system is regulated and compare the regulation under normal circumstances to the pathogenic circumstance. To accomplish this, we sought to (1) identify new factors that are involved in regulating the blood-clotting process, (2) understand how the proteins function in the control of the process, (3) understand how the genes are regulated, (4) examine the influence of defects in the function of the proteins on the human disease process, (5) examine the influence of inhibition of the function of the proteins in animal models of human disease, (6) use crystallographic and biophysical techniques to determine the molecular structure of the proteins and complexes, and (7) determine how the regulatory proteins of the coagulation system control inflammation, and vice versa.
Work from our laboratory and from many others has shown that hereditary tendencies toward developing venous thrombosis are most commonly the result of defects in the proteins that participate in the protein C anticoagulant pathway. These proteins are also involved in protection from the deleterious effects of bacterial infection (a process leading to septic shock) of the bloodstream, where the engagement of the protein C anticoagulant pathway is critical to the survival of the patients. Studies were aimed at elucidating how the pathway protects the individual from septic shock. Earlier we demonstrated that activated protein C (APC) could protect animals, including nonhuman primates, from the lethal effects of Escherichia coli infusion. APC was shown to block coagulation induced by E. coliinfusion, facilitate clot lysis, and limit cytokine elaboration. As such, it was uniquely poised to serve as a candidate for the treatment of severe sepsis in humans, a disease that has a mortality rate of approximately 30-50 percent. A recent phase III trial conducted by Eli Lilly confirmed this hypothesis and demonstrated a decrease of approximately 20 percent in the death rate of severe sepsis patients given APC (this drug is now called Xigris). These clinical results provided impetus to establish the multiple modes of action by which APC accomplishes this function. My laboratory studyied the multiple modes of action that make APC effective as a therapy for inflammatory diseases like sepsis. Greater understanding of these mechanisms is likely to generate new diagnostic and therapeutic approaches.
The newest member of the protein C pathway, the endothelial protein C receptor (EPCR), was identified in our laboratory, but the influence of the receptor on the shock process was unknown. Blocking the ability of the receptor to function results in dramatically increased sensitivity to bacterial infusion, resulting in increased blood clotting, increased inflammation, and vascular degeneration. At least part of this function is manifested because of an unexpectedly strong contribution of EPCR to protein C activation. We have deleted the EPCR gene in mice and have shown that this deletion leads to a hypercoaguable phenotype that is also highly sensitized to death from septic shock. In the deficient mice, inflammation and loss of vascular integrity play dominant roles in their hypersensitivity to inflammatory challenges.
EPCR has an additional unusual property: it can traffic from the plasma membrane and carry APC as cargo. This trafficking appears to alter the expression of a subset of genes. These properties suggested that EPCR plays a critical role in development. This was borne out when deletion of the gene in mice caused an early embryonic lethal phenotype (about embryonic day 8.5). Replacement of wild-type EPCR in mice with specific mutations designed to block single EPCR functions is in progress to elucidate the physiological significance of each of the functions described above.
A complete understanding of how the blood-clotting process is regulated requires an appreciation of the structure of the proteins involved in the process, both alone and in the complexes responsible for their biological activity. Our group solved the crystal structure of EPCR bound to a portion of protein C. The structure confirmed the prediction from the primary sequence that EPCR is structurally very similar to the major histocompatibility complex class I family of molecules. Binding to protein C, however, involves a region of EPCR distinct from the antigen-binding groove found in the class I proteins. A tightly bound lipid (primarily phosphatidylcholine) is, however, present in this groove. Current studies indicate that EPCR deficient mice develop anti-phospholipid antibodies and that these antibodies have significant inhibitory effects on the activated protein C anticoagulant properties. The latter finding probably contributes to the propensity of patients with these antibodies to develop arterial, venous and microvascular blood clots.
When blood vessels are injured, as occurs in angioplasty, the vascular response for the vessel wall is for the cells to proliferate (restenosis). The resultant narrowing of the blood vessel contributes to the requirement to repeat the procedure. In mice, they have found that modulation of the protein C pathway can decrease this vascular thickening dramatically. These results suggest a new approach to treating a common clinical problem.
Together, these studies should improve our understanding of the blood-clotting process in health and disease.
Research
Blood clots may cause heart attacks, strokes, pulmonary emboli and venous thrombosis. They contribute to mortality and morbidity in septic shock, acute trauma injury and complications of diabetes. Our laboratory primarily studied blood clotting and its relationship to inflammation.
We sought to identify factors regulating blood clotting and determine their function. We also investigated clotting protein defects in human disease, clotting protein function in animal models of human disease, structures of clotting proteins and complexes by crystallographic and biophysical techniques, relationships between coagulation and inflammation and regulation of clotting genes.
Proteins of the protein C anticoagulant pathway protect against septic shock, and we investigated activated protein C (APC) protection from lethal effects of Escherichia coli infusion in nonhuman primates. APC blocked E. coli induced coagulation, facilitated clot lysis and limited cytokine elaboration, presenting itself as a candidate for treatment of severe sepsis. A phase III trial conducted by Eli Lilly confirmed that APC effectively treats sepsis and it is now marketed as Xigris. These results provide impetus to establish the numerous mechanisms of APC function. We identified the endothelial protein C receptor (EPCR) and are investigating its function. Blocking receptor function increases sensitivity to bacterial infusion, blood clotting, inflammation and vascular degeneration. We showed that this is partly due to EPCR’s contribution to protein C activation, as hypercoagulation correlating with septic shock lethality occurred in mice lacking the EPCR gene. Mutations to block specific EPCR-functions are in progress.
Structures of clotting proteins and complexes must be solved to fully understand clotting regulation and potential therapies. We solved the crystal structure of EPCR bound to a portion of protein C, showing a requirement for a bound lipid. EPCR deficient mice develop anti-phospholipid antibodies that inhibit activated protein C anticoagulation. We suspect that this contributes to abnormal blood clotting in patients with these antibodies.
Blood vessel injuries, such as in angioplasty, cause cell proliferation and narrowing of vessel diameter and necessitate additional procedures. We found that modulating the protein C pathway in mice decreases vascular damage, suggesting this as a therapy.
Brief CV
Education
B.S., University of Illinois, 1969
Ph.D., Washington University, St. Louis, MO, 1973
Honors and Awards
1974-1976 National Institutes of Health Postdoctoral Fellowship, University of Wisconsin
1977-1979 John L. Dickinson Memorial Award, American Heart Association
1980-1985 Established Investigator Award, American Heart Association
1983 The Merrick Award for Outstanding Research, OMRF
1983 Distinguished Investigator Award for Contributions to Hemostasis, IXth International Congress on Thrombosis and Haemostasis, Stockholm, Sweden
1985-1995 Merrick Distinguished Scientist, OMRF
1988 M.E.R.I.T. Award, National Heart, Lung and Blood Institute
1988 Investigator, Howard Hughes Medical Institute
1989 Chairman, Gordon Conference on Hemostasis
1990 First Sol Sherry Lecturer in Thrombosis, American Heart Association
1995 E. Donnall Thomas Lecture and Prize, American Society of Hematology
1996 Lloyd Noble Chair in Cardiovascular Research, OMRF
1999 Distinguished Career Award, Biennial Awards for Contributions to Hemostasis, XVII Congress of International Society on Thrombosis and Haemostasis
2001 Edward L. and Thelma Gaylord Prize for Scientific Achievement, OMRF
2002 Inaugural member, Oklahoma Inventors Hall of Fame
2002 Membership, National Academy of Sciences
2004 Member, Advisory Council, National Heart, Lung & Blood Institute, NIH
2005 Participant, 6th Annual Public Interest Organization Meeting
2005 Participant, Board of Extramural Advisors Meeting, NHLBI
2005 Editorial board member, Proceedings of National Academy of Science (USA)
2009 Ruysch Lecture, Discoveries that make a difference, Academic Medical Center, Amsterdam, The Netherlands
2009 Plenary Lecture, European Hematology Association, Berlin, Germany
2009 Honored by Journal of Biological Chemistry, Kresge N, Simoni RD, Hill RL. JBC Classics: Blood clotting and the isolation of factor V: The work of Charles T. Esmon. J Biol Chem 284:e2-e3, 2009.
2010 Elected as Honorary Member, American Society of Clinical Investigation
2010 Recipient, Basic Research Prize, American Heart Association
2011-2014 Member, Scientific Review Board, SMARTT (Science Moving towards Research Translation and Therapy) Program, National Heart, Lung & Blood Institute, NIH
Other Activities
Editorial boards of numerous scientific journals; faculty for courses in coagulation and thrombosis at the University of Oklahoma Health Sciences Center; advisory and review committees for American Heart Association, FASEB, Gordon Conferences, NIH, numerous universities, biotechnology companies, hospitals and professional societies; invited lecturer at conferences and meetings throughout the world.
Joined OMRF Scientific Staff in 1982
Publications
Recent Publications
Jiang M, Yang F, Jiang Y, Cheng L, Han J, Yi J, Zuo B, Huang L, Ma Z, Li T, Cao L, Xia Z, Bai X, Jia C, Yang TTC, Esmon NL, Ruan C, Xia L, Esmon C, Han Y, Wu D, Xu J. Safety and efficacy of anti-human activated protein C antibody SR604 for prophylaxis of congenital factor deficiencies. Blood, 2023 June, PMID: 37294924
Jiang M, Yang F, Jiang Y, Cheng L, Han J, Yi J, Zhang G, Ma Z, Cao L, Zuo B, Zhou L, Huang L, Niu S, Xia Z, Zhou X, Bai X, Esmon NL, Ruan C, Xia L, Han Y, Esmon C, Wu D, Xu J. Blocking human protein C anticoagulant activity improves clotting defects of hemophilia mice expressing human protein C. Blood Adv, 2022 April, PMID: 35390147, PMCID: PMC9198932
Ye J, Esmon CT. Factor Xa-factor Va complex assembles in two dimensions with unexpectedly high affinity: an experimental and theoretical approach. Biochemistry 34:6448-53, 1995 May, PMID: 7756276
Selected Publications
Gur-Cohen S, Kollet O, Graf C, Esmon CT, Ruf W, Lapidot T. Regulation of long-term repopulating hematopoietic stem cells by EPCR/PAR1 signaling. Ann N Y Acad Sci. 2016 Apr;1370(1):65-81. Epub 2016 Mar 1. PMID: 26928241 PMCID: PMC5193365
Lattenist L, Jansen MP, Teske G, Claessen N, Meijers JC, Rezaie AR, Esmon CT, Florquin S, Roelofs JJ. Activated protein C protects against renal ischaemia/reperfusion injury, independent of its anticoagulant properties. Thromb Haemost. 2016 Jul 4;116(1):124-33. Epub 2016 Apr 7. PMID: 28687614
Shaw MA, Kombrinck KW, McElhinney KE, Sweet DR, Flick MJ, Palumbo JS, Cheng M, Esmon NL, Esmon CT, Brill A, Wagner DD, Degen JL, Mullins ES. Limiting prothrombin activation to meizothrombin is compatible with survival but significantly alters hemostasis in mice. Blood. 2016 Aug 4;128(5):721-31. PMID: 27252233 PMCID: PMC4974202
Cohen SG, Itkin T, Chakrabarty S, Graf C, Kollet O, Ludin A, Golan K, Kalinkovich A, Ledergor G, Wong E, Niemeyer E, Porat Z, Erez A, Sagi I, Esmon CT, Ruf W, Lapidot T. PAR1 signaling regulates the retention and recruitment of EPCR-expressing bone marrow hematopoietic stem cells. Nat Med. 2015 Nov;21(11):1307-17. Epub 2015 Oct 12. PMID: 27252233 PMCID: PMC4776769
Ogbechi J, Ruf MT, Hall BS, Bodman-Smith K, Vogel M, Wu HL, Stainer A, Esmon CT, Ahnstrom J, Pluschke G, Simmonds RE. Mycolactone-dependent depletion OF endothelial cell thrombomodulin is strongly associated with fibrin deposition in Buruli ulcer lesions. PLoS Pathog. 2015 Jul 16;11(7):e1005011. PMID: 26181660 PMCID: PMC4504485
Sampath S, Brazier AJ, Avril M, Bernabeu M, Vigdorovich V, Mascarenhas A, Gomes E, Sather DN, Esmon CT, Smith JD. Plasmodium falciparum adhesion domains linked to severe malaria differ in blockade of endothelial protein C receptor. Cell Microbiol. 2015 Dec;17(12):1868-82. PMID: 26118955 PMCID: PMC4661071
Contact
Coagulation Biology Laboratory, MS 51
Oklahoma Medical Research Foundation
825 N.E. 13th Street
Oklahoma City, OK 73104
Phone: (405) 271-6474
Fax: (405) 271-2870
E-mail: Charles-Esmon@omrf.org
For media inquiries, please contact OMRF’s Office of Public Affairs at news@omrf.org.
News from the Esmon lab

A patent provides its owner with an exclusive right to a new invention. And beginning in the 1990s, the U.S. Patent and Trademark Office granted a multitude to OMRF, sometimes more than a dozen in a single year. Only a decade earlier did Congress give OMRF and others the right to patent inventions that stemmed […]
A drug based on discoveries made at OMRF was honored today at the National Press Club in Washington, DC. Each year, the National Organization for Rare Disorders honors individuals and companies for outstanding contributions toward improving the lives of people affected by rare diseases. This year, the group recognized Ceprotin, developed from the work of […]
On Saturday, University of Central Oklahoma senior Meagan McLain will walk across the stage at commencement. The 24-year-old will shake hands, receive her diploma and toss her cap in the air. And with her newly minted degree in marketing, she’ll think of all that lies ahead for her: a career, a family, a life. But […]

Top cardiovascular researchers from around the world will converge in Oklahoma City this week to discuss advances and emerging therapies for thrombosis, a primary cause of heart disease. The Oklahoma Medical Research Foundation, home to some of the world’s experts in this field, will play host to the Thrombosis Symposium on May 29. The event […]
When Dr. Charles Esmon began studying activated protein C in the 1970s, he never imagined his work would lead to a pair of life-saving drugs. “Back then, we didn’t even know what activated protein C did in the body,” said the Oklahoma Medical Research Foundation scientist. “Our goal was to figure it out.” Figure it […]
Rayna DuBose came to say thank you. And thank you and thank you and thank you. “OMRF, the scientists and doctors—it’s good to meet the people who helped save me,” she said. “I just wanted to say thank you. I can’t say it enough.” DuBose, a 24-year-old Virginian, spoke Tuesday to more than 100 Oklahoma […]
The U.S. Food and Drug Administration (FDA) has approved a new drug that has its origins at the Oklahoma Medical Research Foundation as the first biologic treatment for patients with a rare genetic defect that can cause a potentially life-threatening clotting disorder. The drug is a treatment for patients with complications related to severe congenital […]
At its annual honors and awards banquet this evening, the Oklahoma Medical Research Foundation will name a pair of scientists as endowed chairs and add two new members to its board of directors. Xiao-Hong Sun, Ph.D., will be installed as the Eli Lilly Distinguished Chair in Biomedical Research, while Gary Gorbsky, Ph.D., will become the […]
The law firm of Kilpatrick Stockton has made a $100,000 contribution to the Oklahoma Medical Research Foundation (OMRF), the organizations announced today. Kilpatrick Stockton’s substantial gift will help OMRF establish a magnetic resonance imaging (MRI) facility for mice, the first of its kind in Oklahoma. The new facility, which will be completed in 2004, will […]
The Oklahoma Medical Research Foundation announced today that Fletcher B. Taylor, Jr., M.D., who has spent more than two decades as a scientist at OMRF, has endowed a chair at the foundation. Taylor’s gift will establish the Alvin Chang Chair in Cardiovascular Biology. The chair is named in honor of Taylor’s longtime senior research assistant, […]
The Oklahoma Medical Research Foundation announced today that it has received a $10 million grant from the National Institutes of Health. “This is yet another important step in the emergence of Oklahoma as a center of biomedical excellence,” said OMRF President Dr. J. Donald Capra. “Five years ago, this state had never seen a $10 […]
The Oklahoma Medical Research Foundation (OMRF) and Eli Lilly and Company (NYSE:LLY) are pleased to announce that they have resolved a lawsuit pending between them in federal court in Oklahoma City involving Lilly’s life saving drug, Xigris®. The terms of the settlement are confidential but it will enable OMRF and Lilly to continue to collaborate […]
An Oklahoma Medical Research Foundation scientist has become only the fourth Oklahoman in history to be elected to the National Academy of Sciences. After the Nobel Prize, membership in the Academy is one of the highest honors that can be accorded to a scientist. Dr. Charles T. Esmon, OMRF Lloyd Noble Chair in Cardiovascular Research, […]
An Oklahoma City federal court ruled Wednesday that the Oklahoma Medical Research Foundation may proceed with legal action against pharmaceutical giant Eli Lilly and Company for patent infringement, fraud, constructive fraud and unjust enrichment. The lawsuit involves a treatment for severe sepsis, sometimes referred to as “blood poisoning”, which kills more than 215,000 people each […]
Oklahoma City, OK – The Oklahoma Medical Research Foundation announced that Len Cason has been elected Chairman of the Board of Directors during its annual meeting today. Cason has been an attorney with the Oklahoma City firm of Hartzog Conger Cason and Neville for the past thirteen years. He has been a member of OMRF’s […]
“From Bench to Bedside: Biomedicine at the New Millenium,” a series of free public lectures this fall sponsored by the Oklahoma Medical Research Foundation, will feature nationally and internationally recognized OMRF scientists and physicians presenting the lastest research being done on a number of high profile diseases and conditions. “These exciting and informative programs are […]